Precision and Accuracy in 2025: A Strategic Guide to Pharmaceutical Method Validation and Verification
This article provides researchers, scientists, and drug development professionals with a comprehensive guide to navigating the evolving landscape of analytical method validation and verification in 2025.
Precision and Accuracy in 2025: A Strategic Guide to Pharmaceutical Method Validation and Verification
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive guide to navigating the evolving landscape of analytical method validation and verification in 2025. It covers foundational principles grounded in ICH Q2(R2) and Q14, explores modern methodological applications including Quality-by-Design (QbD) and AI-driven analytics, addresses common troubleshooting and optimization challenges, and offers a clear comparative analysis of validation versus verification strategies. The content synthesizes current regulatory trends, technological innovations, and practical frameworks to ensure robust, compliant, and efficient analytical practices in pharmaceutical development.
The Pillars of Reliability: Understanding Accuracy, Precision, and Regulatory Foundations
In pharmaceutical development and quality control, analytical methods must be reliable, reproducible, and fit for their intended purpose. Method validation provides assurance that analytical procedures consistently produce reliable results, with Accuracy, Precision, Specificity, and Linearity representing fundamental performance characteristics required by global regulatory standards [1] [2]. These parameters form the foundation for ensuring the credibility of scientific data supporting drug identity, strength, quality, purity, and potency [3].
The International Council for Harmonisation (ICH) guideline Q2(R1) establishes a comprehensive framework for validating analytical procedures, with the United States Pharmacopeia (USP), Japanese Pharmacopoeia (JP), and European Union (EU) guidelines maintaining close alignment with these core principles [2]. This guide objectively compares these essential parameters based on established regulatory requirements and experimental approaches.
Core Parameter Definitions and Regulatory Context
Regulatory Framework Comparison
While harmonized in principle, minor differences exist in how regulatory bodies approach method validation:
Table 1: Regulatory Terminology Comparison
| Parameter | ICH Q2(R1) | USP <1225> | JP Chapter 17 | EU Ph. Eur. 5.15 |
|---|---|---|---|---|
| Intermediate Precision | Intermediate Precision | Ruggedness | Intermediate Precision | Intermediate Precision |
| System Suitability | Implied | Emphasized | Strong emphasis | Emphasized |
| Robustness | Included | Included | Strong emphasis | Strong emphasis |
All guidelines emphasize science and risk-based approaches, allowing flexibility based on method intent [2]. USP particularly focuses on compendial methods and system suitability testing, while JP and EU place greater emphasis on robustness [2].
Parameter Definitions
Accuracy: The closeness of agreement between test results obtained by the method and the true value or an accepted reference value [1] [4]. It measures systematic error and is typically reported as percentage recovery [4].
Precision: The closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions [1] [5]. It measures random error and is considered at three levels: repeatability, intermediate precision, and reproducibility [4].
Specificity: The ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [1] [2]. For identification tests, specificity ensures identity; for assay and impurity tests, it ensures separation from interfering substances [1].
Linearity: The ability of the method to obtain test results directly proportional to the concentration of analyte in the sample within a given range [1] [4]. It demonstrates the method's capacity to elicit proportional responses to concentration changes [5].
Experimental Protocols and Assessment Methodologies
Accuracy Assessment Protocols
Drug Substance Assays:
- Use analyte of known purity (reference material or well-characterized impurity)
- Compare experimental concentration against theoretical concentration
- Alternative approach: Compare results with orthogonal procedure using distinct measurement approach [4]
Drug Product Assays:
- Spike known quantity of analyte into synthetic matrix containing all components except analyte
- If difficult to recreate all components, spike known amounts into actual test sample
- Compare results between unspiked and spiked samples [4]
Impurity Quantitation:
- Spike samples with known amounts of impurities
- If impurity references unavailable, compare with independent procedure or use drug substance response factor [4]
Experimental Design: Assess using minimum 3 concentration points covering reportable range with 3 replicates each. Perform complete analytical procedure for every replicate [4].
Case Study - Accuracy in Practice: An HPLC investigation of cranberry anthocyanins demonstrated how accuracy depends on calibration approach. When cyanidin-3-glucoside served as calibrant for all compounds, accuracy varied significantly compared to using individual anthocyanin reference standards, highlighting the importance of appropriate reference materials [3].
Precision Evaluation Methods
Repeatability:
- Minimum 9 determinations (3 concentrations × 3 replicates) covering reportable range, OR
- Minimum 6 determinations at 100% test concentration [4]
- Express as standard deviation, relative standard deviation, and confidence interval [4]
Intermediate Precision:
- Assess variations within same laboratory
- Include different days, different analysts, different equipment, different environmental conditions [4]
- Objective: Verify method provides consistent results after development phase [4]
Reproducibility:
- Demonstrate precision between different laboratories
- Critical for pharmacopoeial method standardization [4]
Precision Acceptance Criteria: The Horwitz equation provides empirical guidance for acceptable precision: RSDr = 2C^-0.15 where C is concentration as mass fraction [5]. The modified Horwitz values for repeatability include:
Table 2: Horwitz-Based Precision Standards
| Analyte Percentage | Acceptable %RSD (Repeatability) |
|---|---|
| 100.00% | 1.34% |
| 50.00% | 1.49% |
| 20.00% | 1.71% |
| 10.00% | 1.90% |
| 5.00% | 2.10% |
| 1.00% | 2.68% |
| 0.25% | 3.30% |
Specificity Demonstration
For chromatographic methods, specificity is established by:
- Examining chromatographic blanks in expected analyte retention time window [5]
- Demonstrating baseline separation between analyte and potential interferents
- For assay methods, demonstrating no interference from placebo or matrix components
- For impurity methods, resolving all potential impurities and degradation products [1]
Linearity and Range Determination
Linearity Experimental Protocol:
- Prepare series of standard solutions at minimum 5 concentration levels
- Distribute concentrations appropriately across working range (typically 50-150% of expected range) [5]
- Analyze each concentration minimum twice [5]
- Plot concentration versus response
- Calculate regression line by method of least squares [4]
Range Establishment: The specific range depends on method application:
Table 3: Method-Specific Range Requirements
| Test Method | Acceptable Range |
|---|---|
| Drug Substance/Product Assay | 80-120% test concentration |
| Content Uniformity | 70-130% test concentration |
| Dissolution Testing | ±20% over specification range |
| Impurity Assays | Reporting level to 120% specification |
Acceptance Criteria: For linear regression, typically requires R² > 0.95, though non-linear methods may be validated with different statistical approaches [4].
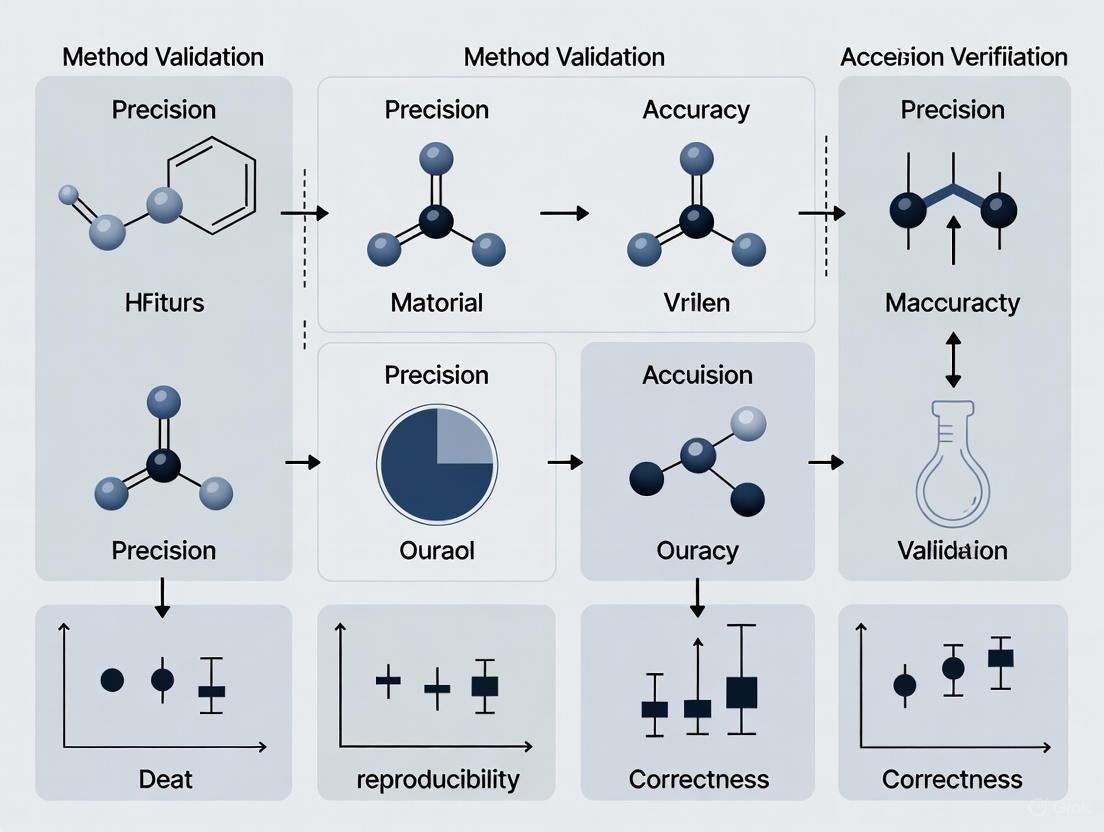
Method Validation Workflow and Relationships
The validation process follows a logical sequence where parameters build upon each other to establish method reliability.
Figure 1: Method Validation Parameter Workflow
Accuracy Assessment Methodologies
Different approaches to accuracy determination provide complementary verification of method reliability.
Figure 2: Accuracy Verification Approaches
Essential Research Reagent Solutions
Table 4: Key Reagents and Materials for Validation Studies
| Reagent/Material | Function in Validation | Critical Specifications |
|---|---|---|
| Reference Standards | Quantitation, identification, calibration curve establishment | Certified purity, stability, proper storage conditions [3] |
| Matrix Components | Placebo/excipient mixtures for specificity and accuracy | Represents final product composition, free of target analyte |
| Spiking Solutions | Known concentration solutions for recovery studies | Precise concentration, stability-matched with analyte [4] |
| Chromatographic Blanks | Specificity demonstration, interference assessment | Contains all components except target analyte [5] |
| System Suitability Standards | Verify chromatographic system performance | Resolution, tailing factor, precision, theoretical plates |
Detection and Quantitation Limit Determination
For methods requiring sensitivity assessment, Detection Limit (DL) and Quantitation Limit (QL) represent critical parameters:
Signal-to-Noise Approach:
- DL: Signal-to-noise ratio of 3:1 [4] [5]
- QL: Signal-to-noise ratio of 10:1 [4] [5]
- Suitable for methods with baseline noise measurement capability [4]
Standard Deviation and Slope Method:
- DL = (3.3 × σ)/S [5]
- QL = (10 × σ)/S [4] [5]
- Where σ = standard deviation of response, S = slope of calibration curve [5]
Visual Evaluation: Non-instrumental methods may use visual determination of minimal detectable or quantifiable levels [1].
Table 5: Core Parameter Acceptance Criteria Summary
| Parameter | Experimental Requirement | Typical Acceptance Criteria | Regulatory Reference |
|---|---|---|---|
| Accuracy | 3 concentrations, 3 replicates each | Recovery: 98-102% (drug substance), spiked recovery within specified range | ICH Q2(R1), USP <1225> [2] [4] |
| Precision (Repeatability) | 6 determinations at 100% or 9 across range | RSD ≤ 1-3% depending on concentration | Horwitz Equation [5] |
| Specificity | Chromatographic blanks, resolution mixtures | No interference at retention time, baseline separation | ICH Q2(R1) [1] [2] |
| Linearity | Minimum 5 concentration points | R² > 0.95 (or appropriate non-linear fit) | ICH Q2(R1) [4] |
| Range | Derived from linearity studies | Method-dependent (see Table 3) | ICH Q2(R1) [4] |
The core parameters of Accuracy, Precision, Specificity, and Linearity provide the foundational framework for demonstrating analytical method validity. While implementation details may vary slightly across regulatory jurisdictions, the fundamental requirements remain consistent globally. Through systematic experimental protocols and appropriate acceptance criteria, these parameters collectively ensure that analytical methods generate reliable, reproducible data suitable for regulatory decision-making in pharmaceutical development and quality control.
The International Council for Harmonisation (ICH) Q2(R2) and ICH Q14 guidelines represent a significant evolution in the regulatory approach to analytical procedures. Effective from 14 June 2024, these documents form a cohesive framework that transitions from a one-time validation exercise to an integrated Analytical Procedure Lifecycle Management (APLM) approach [6]. ICH Q2(R2) focuses on the "validation of analytical procedures," providing a framework for demonstrating that a method is fit for its intended purpose, while ICH Q14 outlines science and risk-based approaches for "analytical procedure development" [7] [8].
This harmonized guidance, adopted by both the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), aims to improve regulatory communication and facilitate more efficient, science-based approval and post-approval change management [6]. For researchers and drug development professionals, understanding this integrated framework is crucial for developing robust, reliable methods that ensure product quality throughout their lifecycle.
Detailed Comparison: ICH Q2(R1) vs. ICH Q2(R2)
The revision from Q2(R1) to Q2(R2) introduces key changes to accommodate modern analytical technologies and align with the principles of ICH Q14.
Key Terminology and Structural Updates
The revised guideline incorporates several important conceptual shifts to address both chemical and biological analytical procedures [6]:
- Linearity is replaced by "Reportable Range" and "Working Range": The "Working Range" consists of "Suitability of calibration model" and "Lower Range Limit verification". This change better accommodates non-linear analytical procedures commonly used for biologics [6].
- Expanded Scope: ICH Q2(R2) now explicitly includes validation principles for analytical procedures using spectroscopic or spectrometry data (e.g., NIR, Raman, NMR, MS), which often require multivariate statistical analyses [6].
- Lifecycle Integration: The guideline explicitly allows for suitable data derived from development studies (per ICH Q14) to be used as part of the validation data, breaking down the traditional silos between development and validation [6].
Comparative Analysis of Validation Characteristics
The following table summarizes the core changes in validation requirements between ICH Q2(R1) and the new Q2(R2) framework:
Table 1: Comparison of Analytical Validation Requirements between ICH Q2(R1) and ICH Q2(R2)
| Validation Characteristic | ICH Q2(R1) Requirements | ICH Q2(R2) Updates | Impact on Method Validation |
|---|---|---|---|
| Linearity/Range | Defined as linearity across specified range | Replaced by "Reportable Range" & "Working Range"; includes calibration model suitability | Better accommodates non-linear methods for biologics |
| Scope of Application | Primarily chromatographic methods | Expanded to include multivariate methods (NIR, Raman, NMR, MS) | Supports modern analytical technologies |
| Development Data Utilization | Validation typically separate from development | Development data (ICH Q14) can be incorporated into validation | Reduces redundant testing; promotes knowledge-based approach |
| Platform Procedures | Not explicitly addressed | Reduced validation testing allowed for established platform methods | Increases efficiency for well-understood technologies |
| Lifecycle Approach | Implicit in quality by design (QbD) | Explicitly integrated with ICH Q14 for full procedure lifecycle | Encourages continuous improvement and knowledge management |
The Synergy between ICH Q14 and ICH Q2(R2)
ICH Q14, "Analytical Procedure Development," provides the scientific foundation that complements the validation principles in ICH Q2(R2). This guideline describes "science and risk-based approaches for developing and maintaining analytical procedures" suitable for assessing the quality of drug substances and products [8]. The enhanced approach in ICH Q14 facilitates improved communication between industry and regulators, providing a more structured framework for submitting analytical procedure development information [9].
Together, ICH Q2(R2) and ICH Q14 cover the development and validation activities used to assess product quality throughout the lifecycle of an analytical procedure, creating a seamless transition from initial development to ongoing monitoring and improvement [6]. This integrated approach is designed to support more flexible and efficient post-approval change management, potentially reducing regulatory submissions for minor changes [6].
FDA and EMA Implementation Timelines and Expectations
Both the FDA and EMA have adopted these guidelines, demonstrating global regulatory harmonization.
Adoption and Implementation Timeline
The FDA announced the availability of both ICH Q2(R2) and ICH Q14 guidelines in March 2024, confirming they were "prepared under the auspices of the International Council for Harmonisation" [7]. The EMA had previously published the new ICH Q14 as Step 5 in January 2024, with the effective date of 14 June 2024 [7]. This synchronized implementation underscores the commitment to global regulatory alignment.
Regulatory Emphasis and Focus Areas
While both agencies have adopted the same guidelines, their historical approaches to process validation provide context for their implementation focus:
- FDA's Approach: Traditionally emphasizes a three-stage model for process validation (Process Design, Process Qualification, and Continued Process Verification) with high emphasis on statistical process control [10].
- EMA's Approach: Outlined in Annex 15 of the EU GMP Guidelines, it maintains a lifecycle focus but with greater flexibility in ongoing verification approaches [10].
Despite these historical differences, the adoption of ICH Q2(R2) and Q14 represents a significant harmonization achievement. Both agencies now expect manufacturers to implement the science and risk-based approaches outlined in these guidelines, particularly for analytical procedures used in release and stability testing of commercial drug substances and products [6].
Practical Application: Experimental Protocols and Methodologies
Precision Evaluation Protocol
Precision validation remains a cornerstone of analytical method validation, with ICH Q2(R2) maintaining focus on this critical parameter. The Clinical and Laboratory Standards Institute (CLSI) EP05-A2 protocol provides a rigorous approach for determining method precision [11]:
- Experimental Design: The assessment should be performed on at least two levels (e.g., low and high concentrations), as precision can differ across the analytical range. Each level is run in duplicate, with two runs per day over 20 days, with each run separated by at least two hours [11].
- Controls and Conditions: Each run should include quality control samples (different from those used for routine instrument control) and at least ten patient samples to simulate actual operation. The order of analysis should be varied to account for potential sequence effects [11].
- Statistical Analysis: Data should be evaluated for outliers, and precision should be assessed at multiple levels:
- Repeatability (Within-run precision): Closeness of agreement between results under identical conditions over a short time [11].
- Intermediate Precision: Within-laboratory variations due to different days, analysts, or equipment [11].
- Reproducibility: Precision between different laboratories, typically assessed in collaborative studies [11].
The precision is measured as standard deviation (SD) or coefficient of variation (CV%), with the total within-laboratory precision calculated using analysis of variance (ANOVA) components [11].
Analytical Procedure Lifecycle Workflow
The integration of ICH Q14 and Q2(R2) creates a structured workflow for analytical procedures throughout their lifecycle, as illustrated in the following diagram:
Diagram 1: Analytical Procedure Lifecycle Management (APLM) Workflow
This lifecycle approach emphasizes that knowledge gained during routine monitoring and continuous improvement should feed back into procedure development, creating a knowledge management system that supports ongoing method optimization [6].
Essential Research Reagent Solutions for Method Validation
Successful implementation of ICH Q2(R2) and Q14 requires carefully selected reagents and materials. The following table outlines key solutions and their functions in analytical development and validation:
Table 2: Essential Research Reagent Solutions for Analytical Method Validation
| Reagent/Material | Function in Validation | Application Examples |
|---|---|---|
| Reference Standards | Provides accepted reference value for accuracy determination | Drug substance purity qualification; impurity quantification |
| System Suitability Solutions | Verifies chromatographic system performance before analysis | Resolution mixture for HPLC; sensitivity solution for detection limit |
| Quality Control Materials | Monitors assay performance during precision studies | Pooled patient samples; commercial quality control materials |
| Sample Preparation Reagents | Ensconsistent sample processing across validation parameters | Protein precipitation reagents; extraction solvents; derivatization agents |
| Chromatographic Mobile Phases | Maintains consistent separation conditions throughout validation | Buffer solutions; organic modifiers; ion-pairing reagents |
The integrated ICH Q2(R2) and Q14 framework represents a significant advancement in analytical science, moving the industry toward a more holistic, knowledge-driven approach to procedure development and validation. For researchers and drug development professionals, success in this new regulatory environment requires:
- Embracing the lifecycle approach to analytical procedures, from development through retirement
- Implementing science and risk-based principles in procedure development and validation
- Leveraging modern analytical technologies with appropriate validation approaches
- Maintaining comprehensive knowledge management systems to support continuous improvement
With both FDA and EMA adopting these harmonized guidelines, the pharmaceutical industry has an unprecedented opportunity to streamline global development and implement more robust, reliable analytical procedures that ultimately enhance product quality and patient safety.
In regulated research and drug development, the integrity of data is not merely a regulatory expectation but the very foundation upon which reliable scientific conclusions are built. The ALCOA+ framework provides a structured set of principles for ensuring data integrity throughout the data lifecycle. These principles are crucial for method validation, a process that confirms analytical procedures are suitable for their intended use. Without data governed by ALCOA+, the validation of a method's precision, accuracy, and reliability is fundamentally undermined [12] [13].
Originally introduced by the U.S. Food and Drug Administration (FDA) as ALCOA, the concept has been expanded to include additional criteria, forming ALCOA+ [14] [13]. This evolution reflects the growing complexity of data in the pharmaceutical industry and the need for more rigorous data governance. For researchers and scientists, adhering to ALCOA+ is not just about compliance; it is about ensuring that every data point generated during method validation and routine analysis is trustworthy, reproducible, and defensible [12] [15].
The ALCOA+ Principles: Definitions and Regulatory Context
The ALCOA+ acronym encompasses a set of nine core principles that define the attributes of high-integrity data. These principles are recognized globally by major regulatory agencies, including the FDA, the European Medicines Agency (EMA), and the World Health Organization (WHO) [13] [16]. The following table provides a detailed overview of each principle and its significance in a research and development context.
Table 1: The Core Principles of ALCOA+ and Their Application in Research
| Principle | Core Definition | Importance in Method Validation & Research |
|---|---|---|
| Attributable | Data must be traceable to the person or system that generated it, including the source, date, and time [14] [17]. | Ensures accountability for observations and actions during an analytical run, making data traceable to a specific researcher or automated system. |
| Legible | Data must be clear, readable, and permanent for the entire required retention period [14] [16]. | Prevents misinterpretation of critical values, such as sample concentrations or instrument readings, during data review and audit. |
| Contemporaneous | Data must be recorded at the time the activity is performed [14] [17]. | Ensures that observations reflect the true conditions of the experiment, minimizing the risk of errors from reconstructed or memory-based entries. |
| Original | The first or source record of data must be preserved, or a certified true copy must be available [14] [17]. | Protects the authentic record of an experiment, which is the definitive source for verification and review. |
| Accurate | Data must be correct, truthful, and free from errors, with any edits documented and justified [14] [12]. | Fundamental for establishing the precision and trueness of an analytical method during validation studies. |
| Complete | All data, including repeat tests, related metadata, and audit trails, must be present [14] [13]. | Provides the full context of the analytical process, ensuring no critical results are omitted and the dataset is robust for statistical analysis. |
| Consistent | Data should be recorded in a chronological sequence, with all changes documented and time-stamped [14] [16]. | Demonstrates a stable and controlled process over time, which is key for proving method robustness and reproducibility. |
| Enduring | Data must be recorded on durable media and preserved for the entire legally required retention period [14] [17]. | Guarantees that validation data remains available for regulatory inspection, product lifecycle management, and future scientific reference. |
| Available | Data must be readily accessible for review, audit, or inspection throughout its retention period [14] [16]. | Facilitates efficient regulatory submissions, laboratory audits, and the re-analysis of data for investigative purposes. |
The regulatory landscape for data integrity is increasingly harmonizing around these ALCOA+ principles. For instance, the FDA enforces them under CGMP regulations (e.g., 21 CFR Parts 211), while the EMA's Annex 11 explicitly references them for computerized systems [13] [16]. Recent trends show that a majority of FDA warning letters cite data integrity lapses, underscoring the critical non-compliance risks associated with failing to implement ALCOA+ effectively [13].
Experimental Protocols for Verifying Data Accuracy in Analytical Methods
A core objective of method validation is to verify the accuracy of the analytical procedure—how close the measured value is to the true value. The ALCOA principle of "Accurate" data is dependent on the statistical reliability of the measurements generated by the method itself [12]. The following experimental protocol outlines a standard approach for quantifying accuracy, often studied alongside precision.
Protocol for Assessing Method Accuracy and Precision
1. Objective: To determine the accuracy and precision of an analytical method for quantifying an analyte in a specific matrix.
2. Experimental Design:
- Sample Preparation: Prepare a minimum of five samples at three different concentration levels (e.g., 80%, 100%, and 120% of the target concentration) covering the method's range [12].
- Reference Standard: Use a certified reference standard of known purity and concentration to spike the sample matrix.
- Replication: Analyze each concentration level in multiple replicates (a minimum of three, preferably more) to allow for statistical evaluation of precision.
3. Data Collection: Following ALCOA+ principles:
- Attributable & Contemporaneous: Record raw data (e.g., chromatographic peak areas) directly into a laboratory notebook or a validated electronic system (LIMS), with user and timestamp data automatically captured [17] [16].
- Original & Legible: The instrument's original data file is the source record. Any printouts or exported data must be clear and permanently linked to the original file.
- Accurate: Perform system suitability tests (SST) before the analysis to ensure the instrument is functioning correctly [12].
4. Data Analysis:
- Accuracy (Trueness): Calculate the percentage recovery for each sample using the formula:
(Measured Concentration / Theoretical Concentration) * 100. Report the mean recovery and standard deviation for each concentration level [12]. - Precision:
- Repeatability: Calculate the relative standard deviation (RSD) of the replicates within the same day and by the same analyst (intra-day precision).
- Intermediate Precision: Assess the RSD of results generated on different days, by different analysts, or using different equipment (inter-day precision) to gauge the method's robustness [12].
5. Interpretation: The method is considered accurate if the mean recovery at each concentration level falls within a pre-defined acceptance criterion (e.g., 98-102%). Precision is typically acceptable if the RSD is below a threshold, such as 2% for assay methods. The combination of these two metrics provides a comprehensive view of the method's total error [12].
Workflow for Accuracy and Precision Assessment
The following diagram illustrates the logical workflow for planning, executing, and analyzing an experiment to assess the accuracy and precision of an analytical method, incorporating key ALCOA+ checkpoints.
Quantitative Comparison of Data Integrity Approaches
The implementation of ALCOA+ principles can be achieved through different methodologies, primarily paper-based systems, hybrid models, and fully electronic systems. The choice of approach significantly impacts efficiency, error rates, and compliance risk. The following table compares these approaches based on key performance metrics relevant to research and development environments.
Table 2: Performance Comparison of Data Integrity Implementation Approaches
| Implementation Characteristic | Paper-Based System | Hybrid System | Fully Electronic System (with Audit Trail) |
|---|---|---|---|
| Typical Data Entry Error Rate | Higher (Prone to manual transcription errors) [18] | Moderate (Mix of manual and electronic entry) | Lower (Automated data capture from instruments) [19] |
| Efficiency of Data Retrieval | Low (Manual searching of physical archives) | Moderate (Digital search possible for electronic portions) | High (Instant search and filtering across entire dataset) [17] |
| Cost of Regulatory Compliance | High (Manual review, physical storage) | Moderate to High (Management of two systems) | Lower (Automated audit trails, centralized storage) [19] |
| Strength of Audit Trail | Weak (Relies on paper corrections; easily compromised) | Partial (Electronic actions may be logged) | Strong (Comprehensive, immutable log of all actions) [17] [16] |
| Risk of Data Falsification | Higher (Difficult to prove contemporaneity) | Moderate | Lower (Attribution and timestamps are system-enforced) [13] |
| Support for ALCOA+ Principles | Manual, prone to lapses (e.g., legibility, contemporaneity) [17] | Inconsistent (Varies between paper and electronic) | System-enforced and inherent in design [14] [16] |
The Scientist's Toolkit: Essential Reagents and Solutions for Data Integrity
Beyond procedural protocols, ensuring data integrity requires the use of specific, high-quality materials and technical solutions. These tools form the foundation for generating reliable and accurate data in the first place.
Table 3: Essential Research Reagents and Solutions for Data Integrity
| Item | Function in Data Integrity |
|---|---|
| Certified Reference Standards | Provides a traceable and accurate benchmark for calibrating instruments and quantifying analytes, directly supporting the Accurate and Attributable principles [12]. |
| System Suitability Test (SST) Solutions | A standardized mixture used to verify that the entire analytical system (instrument, reagents, columns) is performing adequately before sample analysis, ensuring data Accuracy [12]. |
| Stable Isotope-Labeled Internal Standards | Added to samples to correct for analyte loss during preparation or matrix effects in mass spectrometry, improving the Accuracy and precision of quantitative results. |
| Validated Blank Matrices | Used in bioanalytical method development to prepare calibration standards, ensuring that the measurement is specific to the analyte and free from interference, supporting data Accuracy. |
| Audit Trail Software | A critical technical solution that automatically records all user actions, data creations, modifications, and deletions in a secure, time-stamped log, enforcing Attributable, Contemporaneous, Consistent, and Complete principles [17] [16]. |
| Electronic Lab Notebook (ELN) / LIMS | A centralized software system for managing samples, associated data, and workflows. It structures data entry, controls user access, and maintains records, inherently supporting all ALCOA+ principles [14] [20]. |
The implementation of the ALCOA+ framework is a fundamental prerequisite for any robust method validation and precision-accuracy verification research. It transforms data from mere numbers into reliable, evidence-based knowledge. As the industry moves towards greater digitalization and faces new challenges with complex data types, including those generated by AI, the principles of ALCOA+ remain the constant foundation [19] [13]. For researchers and drug development professionals, embedding these principles into the fabric of daily laboratory practice is not just a regulatory necessity—it is a core component of scientific excellence and a critical factor in bringing safe and effective therapies to patients.
Integrating ICH Q9 Quality Risk Management (QRM) principles into analytical method lifecycle management represents a fundamental shift from reactive compliance to a proactive, science-based framework for ensuring data integrity and product quality. The ICH Q9 guideline, overseen by the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use, provides a systematic process for assessing, controlling, communicating, and reviewing risks that could compromise pharmaceutical product quality [21]. When applied to analytical method lifecycle management—spanning development, validation, routine use, and eventual retirement—this risk-based approach enables organizations to focus resources on method parameters and procedural elements most critical to patient safety and product efficacy.
A robust QRM process, as defined by ICH Q9, is built upon four core components: Risk Assessment, Risk Control, Risk Communication, and Risk Review [22] [21]. This cyclical process ensures that method performance is continuously monitored and maintained throughout its operational lifespan. The recent Q9(R1) revision further strengthens implementation by emphasizing that the degree of formality in risk management should be commensurate with the level of risk, providing crucial guidance for prioritizing efforts based on potential impact to product quality and patient safety [22].
Core Principles of ICH Q9
The Four Components of Quality Risk Management
The ICH Q9 framework establishes a structured, cyclical process for managing quality risks throughout the analytical method lifecycle. This systematic approach ensures consistent application across all stages of method development, validation, and implementation.
Risk Assessment: This foundational component involves a systematic process of risk identification, analysis, and evaluation. It begins with identifying potential hazards or "what could go wrong" with an analytical method, followed by analysis of the potential causes and consequences, and concludes with evaluation against risk criteria [21]. For analytical methods, this typically involves structured tools like Failure Mode Effects Analysis (FMEA) which assesses potential failure modes based on their severity, probability of occurrence, and detectability [22] [21]. The output enables prioritization of high-risk areas requiring immediate control measures.
Risk Control: This component focuses on implementing measures to reduce risks to acceptable levels. Risk control includes risk reduction actions (such as method optimization, additional system suitability tests, or enhanced training) and formal risk acceptance for residual risks that fall within predefined acceptable limits [21]. The Q9(R1) revision specifically emphasizes that risk acceptance decisions must be clearly documented, particularly when they could impact product availability or patient safety [22].
Risk Communication: This ensures transparent sharing of risk management activities, outcomes, and decisions across all relevant stakeholders [21]. For analytical methods, this includes documenting and communicating method limitations, residual risks, and special handling requirements to laboratory analysts, quality assurance, and regulatory affairs personnel. Effective communication ensures all parties understand their roles in maintaining method control.
Risk Review: This final component establishes that risk management is an ongoing process rather than a one-time activity [21]. Regular reviews of method performance metrics—including out-of-specification (OOS) rates, system suitability failure trends, and investigation reports—ensure that risk controls remain effective throughout the method's lifecycle [22]. The review process should be triggered by significant events such as method-related deviations, changes in instrumentation, or transfer to new laboratories.
Key Q9(R1) Revisions and Their Impact
The 2023/2024 revision to ICH Q9 (Q9(R1)) introduced crucial clarifications that directly impact how risk management should be applied to analytical methods, with particular emphasis on managing subjectivity and determining appropriate formality.
Managing Subjectivity: Q9(R1) stresses the need to minimize inherent subjectivity in risk scoring, which directly impacts the reliability of Risk Priority Number (RPN) calculations (Severity × Probability × Detectability) [22]. For analytical methods, this means implementing clearly defined, auditable rating criteria for all elements of the RPN. Regulatory inspectors will challenge QRM outcomes where scoring scales are not consistently applied across different methods or departments. Compliance requires establishing cross-functional QRM teams with representatives from Quality, Process Engineering, Regulatory, and Production to pool expertise and mitigate individual bias [22].
Degree of Formality: The revision mandates that the level of effort, formality, and documentation must correspond to the level of risk to quality and patient safety [22]. This principle is particularly relevant for analytical methods, where the same exhaustive FMEA process should not be applied equally to a compendial method verification and a novel bioanalytical method development. Organizations must define and document a Quality Risk Management Plan that clearly outlines triggers for Formal QRM (requiring cross-functional teams, established tools like FMEA, and standalone reports) versus Informal QRM (using simple techniques with rationale documented within the Quality System) [22].
Table: Determining Level of Formality in Method Risk Management
| Factor | High (Formal QRM Required) | Low (Informal QRM Acceptable) |
|---|---|---|
| Uncertainty | Lack of knowledge about hazards (e.g., new analytical technology, complex OOS) | Good knowledge; easily answer 'what can go wrong' (e.g., minor method adjustment) |
| Importance | High degree of importance relative to product quality (e.g., release method for potency) | Low degree of importance (e.g., in-process test not impacting product quality) |
| Complexity | Highly complex method (e.g., cell-based bioassay, novel technology platform) | Low complexity, well-understood method (e.g., pH measurement) |
Implementing ICH Q9 in Method Lifecycle Management
Method Development and Validation Phase
The integration of QRM begins during method development, where risk assessment tools systematically identify and control variables that could impact method performance. A science-based approach to establishing method acceptance criteria ensures they are fit-for-purpose and proportional to the risk associated with the method's intended use.
Traditional approaches to evaluating method goodness relied heavily on % coefficient of variation (CV) and % recovery, which have significant limitations as they evaluate method performance independent of product specification limits [23]. A modern, risk-based approach instead evaluates method error relative to the product specification tolerance or design margin, answering the critical question: "How much of the specification tolerance is consumed by the analytical method?" [23] This directly links method performance to its impact on out-of-specification (OOS) rates and batch release decisions.
Table: Risk-Based Acceptance Criteria for Analytical Methods
| Validation Parameter | Traditional Approach | Risk-Based Approach (as % Tolerance) | Bioassay Recommendation |
|---|---|---|---|
| Repeatability | % CV relative to mean | ≤ 25% of tolerance | ≤ 50% of tolerance |
| Bias/Accuracy | % Recovery relative to theoretical | ≤ 10% of tolerance | ≤ 10% of tolerance |
| Specificity | Visual demonstration | ≤ 5-10% of tolerance (Excellent-Acceptable) | Similar small % of tolerance |
| LOD | Signal-to-noise ratio | ≤ 5-10% of tolerance (Excellent-Acceptable) | Case-by-case evaluation |
| LOQ | Signal-to-noise ratio | ≤ 15-20% of tolerance (Excellent-Acceptable) | Case-by-case evaluation |
The relationship between method performance and product quality can be mathematically represented to quantify risk. The reportable result from any analytical method is influenced by both the product itself and the method variability [23]:
- Reportable Result = Test sample true value + Method Bias + Method Repeatability [23]
This equation demonstrates that method error directly impacts the ability to make correct batch release decisions. When method variability consumes an excessive portion of the specification range, the probability of OOS results increases significantly, even for products that are truly within specifications [23].
Experimental Protocol: Tolerance-Based Method Validation
A robust, risk-based method validation protocol should incorporate the following elements to ensure method performance is evaluated relative to its impact on product quality decisions:
Sample Preparation: Prepare a minimum of 6 replicates at 100% of target concentration using actual drug product matrix. Include additional samples at 80% and 120% of target to evaluate performance across the specification range [23].
Reference Standard Qualification: Use qualified reference standards with certificates of analysis documenting purity and storage requirements. Include system suitability tests aligned with method capabilities.
Data Collection and Analysis:
- Calculate method repeatability as standard deviation of the 6 replicates
- Compute Repeatability % Tolerance = (Standard Deviation × 5.15)/(USL - LSL) for two-sided specifications [23]
- Compare against the acceptance criterion of ≤ 25% of tolerance (or ≤ 50% for bioassays)
- For accuracy, calculate Bias % of Tolerance = Bias/Tolerance × 100 with acceptance criterion of ≤ 10%
Statistical Evaluation: Establish a Linearity Range using studentized residuals from regression analysis. The method is considered linear as long as studentized residuals remain within ±1.96 boundaries [23].
This tolerance-based approach directly links method validation to product quality risks, enabling science-based justification of acceptance criteria and providing clear understanding of how method performance impacts OOS rates.
Knowledge Management and Ongoing Monitoring
Knowledge Management (KM) serves as the foundation for effective risk-based method lifecycle management, transforming risk assessment from subjective opinion to objective, data-driven decisions [22]. The relationship between KM inputs and QRM outputs creates a continuous improvement cycle that maintains method robustness throughout its operational lifespan.
Table: Knowledge Management Inputs for Method Risk Management
| Knowledge Management Input | QRM Application | Impact on Method Lifecycle |
|---|---|---|
| Annual Product Review (APR) Trends | Assign Probability scores in RPN based on actual historical method failure rates | Replaces subjective estimates with data-driven risk probabilities |
| Method Transfer History | Identifies and re-assesses risks for methods transferred between sites or laboratories | Highlights site-specific implementation risks |
| Deviation and CAPA Effectiveness Data | Verifies that mitigation actions successfully reduced risk as predicted during Risk Review | Demonstrates effectiveness of prior risk control measures |
| Method Development Studies | Provides scientific basis for determining Severity and defining Critical Method Parameters (CMPs) | Establishes proven acceptable ranges for method parameters |
The critical link between knowledge management and risk management becomes evident in the Risk Review phase, where method performance data validates initial risk assessments and drives continuous improvement. Modern electronic Quality Management Systems (eQMS) and Laboratory Information Management Systems (LIMS) enable automated tracking of method performance metrics, creating a living risk profile that updates as new data becomes available [22]. This dynamic approach ensures that method risks are continually re-evaluated based on actual performance rather than remaining static after initial validation.
Comparative Analysis: Traditional vs. Risk-Based Approaches
Experimental Data and Performance Metrics
A comparative analysis of traditional versus risk-based approaches to method lifecycle management reveals significant differences in operational outcomes, regulatory compliance, and resource allocation. The tolerance-based method for establishing acceptance criteria provides a scientifically rigorous framework that directly links method performance to product quality risks.
Table: Performance Comparison of Method Validation Approaches
| Evaluation Parameter | Traditional Approach | Risk-Based Approach | Impact on Quality Decision |
|---|---|---|---|
| Acceptance Criteria Basis | Fixed % RSD/CV regardless of product specifications | % of specification tolerance or margin | Directly links method error to OOS risk |
| Resource Allocation | Uniform intensity across all methods | Scalable effort based on risk priority | 30-50% reduction in low-risk method validation efforts |
| OOS Investigation Rate | Higher false OOS due to inappropriate criteria | Scientifically justified criteria reduce false OOS | 40-60% reduction in unnecessary investigations |
| Method Robustness | Focus on point estimates of performance | Understanding of method capabilities across design space | Improved method transfer success rates |
| Regulatory Flexibility | Limited data to support method adjustments | Science-based justification for changes | Enhanced regulatory confidence for post-approval changes |
Experimental data demonstrates that the risk-based approach significantly improves decision-making throughout the method lifecycle. For example, methods validated using tolerance-based acceptance criteria show a 40-60% reduction in unnecessary OOS investigations without compromising product quality [23]. This reduction stems from properly accounting for method variability within the specification range, rather than treating all method errors as equal regardless of their impact on quality decisions.
The Degree of Formality concept introduced in Q9(R1) enables more efficient resource allocation by matching the rigor of the QRM process to the level of risk [22]. High-complexity methods such as cell-based bioassays or novel technology platforms require formal QRM with cross-functional teams and structured tools like FMEA. In contrast, well-understood compendial methods may only require informal QRM with simplified documentation. This risk-proportionate approach typically reduces validation resources for low-risk methods by 30-50% while strengthening controls for high-risk methods [22].
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing risk-based method lifecycle management requires specific tools and methodologies to effectively identify, assess, and control method risks. The following essential resources form the foundation of a robust QRM program for analytical methods.
Table: Essential Research Reagent Solutions for Method QRM
| Tool/Resource | Function in QRM | Application in Method Lifecycle |
|---|---|---|
| FMEA/FMECA Software | Systematic risk assessment tool for identifying and prioritizing failure modes | Quantifies risk priority numbers (RPN) for method variables; enables data-driven control strategy |
| Statistical Analysis Package | Advanced analytics for method capability assessment and trend analysis | Calculates tolerance-based acceptance criteria; analyzes method robustness across design space |
| Reference Standards | Qualified materials for method accuracy and precision evaluation | Establishes method bias relative to tolerance; supports system suitability testing |
| Design of Experiments (DoE) | Structured approach for understanding method parameter interactions | Maps method design space; identifies critical method parameters requiring tight control |
| Electronic Lab Notebook (ELN) | Documentation platform for risk management activities and decisions | Ensures transparent risk communication; maintains historical risk assessment data |
| Method Validation Protocols | Predefined experimental designs for risk-based method qualification | Standardizes approach to validation; ensures consistent application of QRM principles |
| Stability Testing Systems | Controlled environments for assessing method robustness over time | Provides data for risk review; demonstrates method stability under various conditions |
Integrating ICH Q9 Quality Risk Management into analytical method lifecycle management represents a paradigm shift from standardized compliance to science-based, patient-focused quality assurance. This approach creates a direct linkage between method performance and product quality decisions, enabling organizations to allocate resources effectively while enhancing regulatory confidence. The tolerance-based methodology for establishing acceptance criteria provides a scientifically rigorous framework that acknowledges the real-world impact of method variability on quality decisions.
The Q9(R1) revisions further strengthen this framework by emphasizing appropriate formality and managing subjectivity in risk assessments. When combined with robust knowledge management systems, this creates a dynamic, data-driven approach to method lifecycle management that continuously improves through operational experience. As regulatory authorities increasingly adopt risk-based inspection approaches, organizations with mature QRM integration will benefit from more efficient inspections and greater operational flexibility [22].
For researchers, scientists, and drug development professionals, adopting these risk-based principles represents both a compliance necessity and a strategic opportunity. The resulting methods are not only more robust and reliable but also more economically sustainable throughout the product lifecycle. By building quality into methods through risk-based design rather than relying solely on end-product testing, organizations can achieve higher first-pass success rates, reduce unnecessary investigations, and ultimately deliver safer, more effective medicines to patients.
From Theory to Practice: Modern Method Development and Lifecycle Application
Implementing Quality-by-Design (QbD) in Method Development
The pharmaceutical industry is undergoing a significant transformation in how it ensures product quality, moving away from traditional quality-by-testing approaches toward a more systematic, science-based framework known as Quality by Design (QbD). This paradigm shift, encouraged by regulatory agencies worldwide, emphasizes building quality into products and processes from the beginning rather than relying solely on end-product testing [24]. When applied to analytical method development, the QbD approach creates more robust, reliable, and fit-for-purpose methods that consistently deliver quality data throughout their lifecycle.
The fundamental principle of Analytical Quality by Design (AQbD) is that quality cannot be tested into products but must be designed into the development process. This systematic approach begins with predefined objectives and emphasizes method understanding and control based on sound science and quality risk management [25] [26]. The conventional approach to analytical method validation, which often treats validation as a one-time check-box exercise, is being reimagined through a lifecycle approach that aligns with modern process validation concepts [26]. This article compares the traditional and QbD approaches to method development, providing experimental data and case studies that demonstrate the enhanced performance characteristics of QbD-based methods.
Theoretical Framework: QbD Principles and Terminology
Core Components of the AQbD Framework
The Analytical Quality by Design framework consists of several interconnected components that work together to ensure method robustness and reliability:
Analytical Target Profile (ATP): The ATP is a foundational element that defines the method requirements and performance criteria before development begins. It specifies what the method needs to measure and to what level of performance, including parameters such as precision, accuracy, and sensitivity [26] [27]. The ATP serves as the focal point for all stages of the analytical lifecycle, similar to a user requirement specification for analytical equipment qualification.
Critical Method Attributes (CMAs) and Critical Method Parameters (CMPs): CMAs are the key performance characteristics that must be controlled to ensure the method meets the ATP requirements. CMPs are the variables that significantly impact these attributes [25]. For HPLC methods, typical CMPs include mobile phase composition, buffer pH, column temperature, and flow rate [28].
Method Operable Design Region (MODR): The MODR represents the multidimensional combination and interaction of method variables that have been demonstrated to provide assurance of quality [24]. Operating within the MODR provides flexibility while maintaining method performance.
The Three-Stage Analytical Procedure Lifecycle
A properly implemented AQbD approach follows three distinct stages:
- Stage 1: Method Design - Developing the method based on the ATP through risk assessment and experimental design
- Stage 2: Method Qualification - Demonstrating the method's capability to meet the ATP requirements
- Stage 3: Continued Method Verification - Ongoing monitoring to ensure the method remains in a state of control [26]
This lifecycle approach aligns with the concepts described in USP General Chapter <1220> "Analytical Procedure Lifecycle" and ICH guidelines Q2(R2) and Q14, which provide a modern framework for analytical procedure development and validation [24].
Figure 1: AQbD Workflow showing the systematic relationship between key components across the method lifecycle stages.
Comparative Analysis: Traditional vs. QbD Approach
Fundamental Differences in Philosophy and Implementation
The traditional approach to analytical method development relies heavily on trial-and-error experimentation and one-factor-at-a-time (OFAT) optimization. In contrast, the QbD approach employs systematic, risk-based development with multivariate experimentation [27]. This fundamental difference in philosophy leads to significant variations in methodology, documentation, and long-term performance.
Traditional method development typically focuses on satisfying regulatory requirements as a checklist exercise, with limited understanding of method robustness and ruggedness. The method validation is often treated as a one-time event performed after development is complete, with knowledge transfer to quality control laboratories frequently being problematic [26].
QbD-based method development emphasizes scientific understanding and risk management throughout the method lifecycle. The approach identifies and controls critical method parameters, establishes a method operable design region, and implements continuous verification to ensure ongoing method performance [24].
Table 1: Comprehensive Comparison Between Traditional and QbD-Based Method Development Approaches
| Aspect | Traditional Approach | QbD Approach |
|---|---|---|
| Development Strategy | Trial-and-error, one-factor-at-a-time | Systematic, risk-based, multivariate design |
| Validation Focus | Regulatory compliance, check-box exercise | Method understanding, fitness-for-purpose |
| Knowledge Management | Limited transfer of tacit knowledge | Comprehensive knowledge space definition |
| Robustness Assessment | Often evaluated after validation | Built into development phase using DoE |
| Regulatory Flexibility | Limited, changes require regulatory submission | Enhanced within established design space |
| Lifecycle Perspective | Focus on one-time validation | Continuous verification and improvement |
| Control Strategy | Fixed operating conditions | Flexible within method operable design region |
| Resource Investment | Lower initial investment, potential rework | Higher initial investment, reduced failures |
Impact on Method Performance and Business Outcomes
The QbD approach to analytical method development delivers tangible benefits in method performance and business efficiency. Methods developed using QbD principles demonstrate superior robustness when transferred between laboratories, reduced out-of-specification (OOS) results during routine use, and greater flexibility to accommodate changes in materials or equipment [26].
From a business perspective, the initial investment in systematic development is offset by reduced method failures, fewer investigations, and more efficient technology transfers. Regulatory flexibility within the approved design space also allows for continuous improvement without additional submissions [24] [27].
Experimental Protocols and Case Studies
QbD-Based HPLC Method Development for Treprostinil
A recent study demonstrates the application of AQbD principles to develop a stability-indicating RP-HPLC method for treprostinil, a drug used to treat pulmonary arterial hypertension [25]. The method was developed using a central composite design (CCD) to model the relationship between critical method parameters and observed responses.
Experimental Protocol:
- ATP Definition: The method requirements included separation of treprostinil from degradation products, precise quantification (RSD < 2%), and runtime under 10 minutes.
- Risk Assessment: Initial risk identification using Ishikawa diagram identified flow rate, buffer composition, and column temperature as high-risk factors.
- DoE Implementation: A central composite design was employed with three factors at multiple levels, analyzing responses including retention time, theoretical plates, and tailing factor.
- MODR Establishment: The method operable design region was defined for buffer concentration (0.01N KH₂PO₄), mobile phase ratio (36.35:63.35 v/v buffer:diluent), and column temperature (31.4°C).
- Control Strategy: System suitability tests were established to ensure method performance within the MODR.
Results: The optimized method achieved excellent separation with treprostinil eluting at 2.579 minutes within a 6-minute runtime. The method demonstrated precision (RSD = 0.4%), robustness (RSD < 2%), and effectively separated treprostinil from degradation products under various forced degradation conditions [25].
QbD for Metformin Hydrochloride HPLC Method
Another study applied QbD principles to develop an HPLC method for metformin hydrochloride in tablet dosage forms [29]. The researchers used a two-factor, three-level design with buffer pH and mobile phase composition as independent factors.
Experimental Protocol:
- Factor Screening: Risk assessment identified buffer pH and mobile phase composition as critical parameters.
- Response Surface Methodology: Central composite design was used to study the effects on retention time, peak area, and symmetry factor.
- Optimization: Desirability function was applied to simultaneously optimize multiple analytical attributes.
- Validation: The optimized method was validated according to ICH guidelines.
Results: The optimal conditions consisted of 0.02M acetate buffer (pH 3) and methanol (70:30 v/v) at a flow rate of 1 mL/min. The method was successfully applied for content evaluation and dissolution studies of metformin hydrochloride tablets [29].
Ceftriaxone Sodium HPLC Method Development
A QbD-based approach was also implemented for developing an HPLC method for ceftriaxone sodium in pharmaceutical dosage forms [28]. The researchers applied central composite design to optimize mobile phase composition and pH, with responses including retention time, theoretical plates, and peak asymmetry.
Results: The optimized method used a Phenomenex C-18 column with mobile phase acetonitrile to water (70:30 v/v, pH 6.5 with 0.01% triethylamine) at 1 mL/min flow rate. The method showed excellent linearity (r² = 0.991) across 10-200 μg/mL range, with system suitability parameters within acceptable limits (tailing factor = 1.49, theoretical plates = 5236) [28].
Table 2: Performance Comparison of QbD-Developed HPLC Methods Across Multiple APIs
| Drug Compound | Experimental Design | Optimized Conditions | Method Performance |
|---|---|---|---|
| Treprostinil [25] | Central Composite Design | Buffer (0.01N KH₂PO₄):Diluent (36.35:63.35 v/v), 31.4°C | Retention time: 2.579 min, Precision: 0.4% RSD |
| Metformin HCl [29] | Central Composite Design | Acetate buffer pH 3:Methanol (70:30 v/v), 1 mL/min | Successful application to content uniformity and dissolution |
| Ceftriaxone Sodium [28] | Central Composite Design | Acetonitrile:Water (70:30 v/v), pH 6.5, 1 mL/min | Linearity: r² = 0.991, Tailing factor: 1.49 |
| Remogliflozin Etabonate & Vildagliptin [30] | Box-Behnken Design | 10 mM KH₂PO₄ buffer pH 3:Methanol (10:90 v/v), 0.8 mL/min | %RSD < 2.0, sensitive LOD and LOQ |
| Tafamidis Meglumine [31] | Box-Behnken Design | 0.1% ortho-phosphoric acid in methanol:acetonitrile (50:50 v/v) | Retention time: 5.02 ± 0.25 min, Linearity: R² = 0.9998 |
The Scientist's Toolkit: Essential Reagents and Solutions
Successful implementation of AQbD requires specific reagents, instruments, and software solutions. The following table summarizes key components used in the case studies discussed in this article.
Table 3: Essential Research Reagent Solutions for QbD-Based HPLC Method Development
| Item Category | Specific Examples | Function in AQbD |
|---|---|---|
| Chromatographic Columns | Agilent Express C18, Phenomenex ODS Hypersyl, Cosmosil C18, Qualisil BDS C18 | Stationary phase for separation; column chemistry is a critical method parameter |
| Buffer Systems | Potassium dihydrogen phosphate (KH₂PO₄), Acetate buffer, Ortho-phosphoric acid | Mobile phase component controlling pH and ionic strength; critical for reproducibility |
| Organic Modifiers | HPLC-grade Methanol, Acetonitrile | Mobile phase components affecting retention and selectivity; optimized in DoE |
| Design Software | Design-Expert, Minitab, MODDE | Statistical design and analysis of experiments; enables multivariate optimization |
| HPLC Systems | Agilent HPLC with PDA detector, Waters Alliance Systems, Shimadzu Prominence | Instrument platform; detector selection impacts sensitivity and specificity |
| Column Heaters | Thermostatted column compartments | Control column temperature as critical parameter affecting retention and efficiency |
| pH Meters | Mettler Toledo with combination electrodes | Precise pH adjustment of mobile phases; critical for reproducibility |
| Ultrasonication Baths | Bandelin Sonorex, Branson Ultrasonic | Mobile phase degassing and sample dissolution; prevents bubble formation |
Analytical Method Validation Within QbD Framework
Enhanced Validation Approach
In the QbD paradigm, method validation is not a one-time event but an integral part of the method lifecycle. The enhanced approach focuses on demonstrating that the method is fit-for-purpose based on the predefined ATP [26]. Method qualification (Stage 2) confirms the method's capability to meet the ATP requirements under routine operating conditions.
The validation strategy incorporates knowledge gained during method design, including understanding of the MODR and control strategy. This comprehensive approach typically includes assessment of accuracy, precision, specificity, linearity, range, detection and quantitation limits, and robustness—but with greater scientific rationale behind acceptance criteria [26].
Continued Method Performance Verification
Stage 3 of the method lifecycle involves ongoing assurance that the method remains in a state of control during routine use. This includes continuous monitoring of system suitability test results, periodic assessment of method performance through quality control charting, and investigation of any trends or deviations [26].
The continued verification activities provide data to support method improvements and ensure the method remains fit-for-purpose throughout its lifecycle. This aligns with modern quality systems that emphasize continuous improvement rather than static validation states.
Regulatory Perspective and Future Directions
Evolving Regulatory Landscape
Regulatory agencies worldwide are encouraging the adoption of QbD principles for pharmaceutical development, including analytical methods. The International Council for Harmonisation (ICH) has developed two draft guidelines—ICH Q14 on analytical procedure development and ICH Q2(R2) on analytical procedure validation—that describe QbD principles for analytical methods [24].
The United States Pharmacopeia (USP) has developed General Chapter <1220> "Analytical Procedure Lifecycle" that provides a comprehensive framework for implementing AQbD concepts [24]. This chapter describes a holistic approach for managing the analytical procedure lifecycle and serves as a valuable resource for industry and regulators.
Integration with Green Chemistry Principles
A growing trend in AQbD is the integration of green chemistry principles with method development. Several recent studies have incorporated assessment of method environmental impact using tools such as the Green Analytical Procedure Index (GAPI) and Blue Applicability Grade Index (BAGI) [25] [31].
The treprostinil method development study, for example, reported a GAPI score of 83, classifying the method as environmentally friendly [25]. Similarly, the tafamidis meglumine method achieved an AGREE score of 0.83, indicating high environmental sustainability [31]. This integration of green principles with QbD represents the future of analytical method development in the pharmaceutical industry.
The implementation of Quality-by-Design in analytical method development represents a significant advancement over traditional approaches. The systematic, science-based framework of AQbD results in more robust, reliable, and fit-for-purpose methods that consistently deliver quality data throughout their lifecycle.
Experimental data from multiple case studies demonstrates that QbD-developed methods exhibit superior performance characteristics, including enhanced robustness, reduced method failures, and greater regulatory flexibility. While requiring greater initial investment in development, the AQbD approach ultimately delivers long-term benefits through reduced investigations, more efficient technology transfers, and continuous improvement opportunities.
As the pharmaceutical industry continues to embrace QbD principles, the integration of AQbD with green chemistry concepts and digital transformation initiatives will further enhance the sustainability, efficiency, and reliability of analytical methods. The ongoing evolution of regulatory guidelines supports this paradigm shift, positioning AQbD as the standard for analytical method development in modern pharmaceutical quality systems.
Leveraging Design of Experiments (DoE) for Efficient Optimization
In the rigorous world of pharmaceutical development, establishing robust analytical methods is paramount to ensuring drug safety, efficacy, and quality. Method validation—the process of proving that an analytical procedure is suitable for its intended purpose—relies on definitive evidence of precision, accuracy, and robustness. Traditionally, this was achieved through One-Factor-at-a-Time (OFAT) approaches, which are not only resource-intensive but also fail to detect interactions between critical method parameters [32]. Within this context, Design of Experiments (DoE) has emerged as a superior statistical framework for efficient optimization. DoE is a systematic, multipurpose tool that enables researchers to investigate the simultaneous impact of multiple factors on key analytical responses, thereby building a deep understanding of the method's performance and its limitations [33]. By integrating DoE into method validation strategies, scientists can move beyond simple verification to a state of profound, science-based process knowledge, aligning perfectly with modern regulatory paradigms like Quality by Design (QbD) [34] [35]. This guide objectively compares the performance of different DoE optimization criteria, providing experimental data and protocols to inform researchers and drug development professionals in their pursuit of efficient and reliable method optimization.
Comparative Analysis of DoE Optimization Criteria
Selecting the appropriate optimization criterion is a critical first step in designing an efficient experiment. Different criteria are designed to achieve different primary objectives, such as precise parameter estimation or accurate prediction. The table below provides a structured comparison of the fundamental and advanced DoE optimization criteria to guide this selection.
Table: Comparison of DoE Optimization Criteria and Their Applications
| Criterion | Primary Objective | Key Mathematical Focus | Best-Suited Application in Method Validation |
|---|---|---|---|
| D-optimality | Maximize overall information gain for parameter estimation | Maximize the determinant of the information matrix, ( \max \lvert X^T X \rvert ) [36] | Screening experiments to identify Critical Method Parameters (CMPs) from a large set of variables [33] [36]. |
| A-optimality | Minimize the average variance of parameter estimates | Minimize the trace of the inverse information matrix, ( \min \, \text{tr}[(X^T X)^{-1}] ) [36] | When reliable estimates for all method factors are equally important, and the goal is balanced precision. |
| E-optimality | Control the worst-case variance among parameter estimates | Minimize the maximum eigenvalue of ( (X^T X)^{-1} ) [36] | Ensuring that the least precisely estimated method parameter still meets a pre-defined level of precision. |
| G-optimality | Minimize the maximum prediction variance across the design space | ( \min \, \max_{x \in X} x^T (X^T X)^{-1} x ) [36] | Robustness testing of an analytical method, guaranteeing reliable predictions under worst-case conditions. |
| V-optimality | Minimize the average prediction variance over the design space | ( \min \int_{x \in X} x^T (X^T X)^{-1} x \,dx ) [36] | Optimizing a method for overall reliable performance across its entire operational range. |
| Space-filling | Ensure uniform coverage and exploration of the design space | Geometric and distance-based criteria (e.g., Latin Hypercube) [36] | Developing methods for complex, non-linear processes or when the underlying model is unknown. |
Interpretation of Comparative Data
The choice of criterion involves inherent trade-offs. While D-optimal designs are highly efficient for factor screening, they may not provide uniform precision across the design space [36]. Conversely, A-optimal designs ensure more balanced precision for all parameters but may require more experimental runs to achieve it. For method robustness studies, where proving consistent performance under small, deliberate variations is key (as required by ICH guidelines [37]), G-optimality is particularly valuable as it safeguards against the highest prediction error. When the goal is to establish a Method Operational Design Range (MODR) within a QbD framework, V-optimality or space-filling designs are often preferred for their ability to model the entire method operating space comprehensively [38].
Experimental Protocols for DoE in Analytical Method Validation
The following section outlines detailed methodologies for applying DoE in two common method validation scenarios: a screening experiment and a robustness study.
Protocol 1: Screening Study for an HPLC Method
This protocol aims to identify the Critical Process Parameters (CPPs) affecting the Critical Quality Attributes (CQAs) of a new High-Performance Liquid Chromatography (HPLC) method for drug assay.
- Objective: To identify from a set of five potential factors which ones significantly impact key chromatographic responses (peak area, resolution, and tailing factor).
- Factors and Levels:
- A: Mobile Phase pH (±0.2)
- B: Column Temperature (±5°C)
- C: Flow Rate (±0.1 mL/min)
- D: Gradient Time (±5%)
- E: Detection Wavelength (±5 nm)
- DoE Design Selection: A D-optimal design is selected for its ability to screen many factors with a minimal number of experimental runs, maximizing information gain efficiently [33] [36].
- Experimental Procedure:
- Sample Preparation: Prepare a standard solution of the drug substance and its known impurities in the required matrix.
- DoE Run Execution: Use an automated liquid handler (e.g., dragonfly discovery) to set up the HPLC runs according to the D-optimal design matrix. Automation enhances precision and reproducibility for complex assay setups [39].
- Data Collection: For each experimental run, record the CQAs: Peak Area (for accuracy), Resolution (for specificity), and Tailing Factor (for peak shape).
- Statistical Analysis: Fit a linear model to the data and perform Analysis of Variance (ANOVA) to identify factors and interactions with statistically significant effects (p-value < 0.05) on each response.
Protocol 2: Robustness Testing of a UV-Vis Spectrophotometric Method
This protocol uses a robustness study to demonstrate that a dissolution test method remains unaffected by small, deliberate variations in method parameters.
- Objective: To verify the method's robustness by evaluating the impact of minor parameter changes on the measured absorbance and calculated drug concentration.
- Factors and Levels:
- A: Wavelength (±2 nm)
- B: pH of Buffer (±0.05)
- C: Sonication Time (±10%)
- DoE Design Selection: A Full Factorial design (2³) with 3 center points is used. This design is ideal for robustness testing as it thoroughly explores a defined, narrow factor space and allows for the detection of curvature, providing definitive proof of method resilience [37].
- Experimental Procedure:
- Sample Preparation: Prepare dissolution samples according to the standard procedure.
- DoE Run Execution: Perform the UV-Vis analysis according to the 11-run factorial design (8 factorial points + 3 center points).
- Data Collection: Record the absorbance and the calculated % drug release for each run.
- Statistical Analysis:
- Analyze the main effects and interactions of the factors on the response.
- The method is considered robust if none of the factors show a statistically significant effect on the response at a predetermined significance level (e.g., p > 0.05), and the relative standard deviation (RSD) at the center points is within the acceptance criteria (e.g., <2%) [37].
Workflow Visualization: Implementing DoE for Method Validation
The following diagram illustrates the logical workflow for applying DoE in the context of analytical method development and validation, integrating QbD principles.
DoE Implementation Workflow for Method Validation
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of a DoE requires precise control over experimental conditions and materials. The following table details key reagents and instruments critical for conducting the experimental protocols described in this guide.
Table: Essential Research Reagents and Instruments for DoE Studies
| Item Name | Function / Role in DoE | Critical Specifications |
|---|---|---|
| Pharmaceutical Reference Standards | Serves as the "accepted reference value" for calculating accuracy (%bias/%recovery) [40]. | USP-grade API; certified purity and concentration. |
| Chromatography Columns | The stationary phase for separation; a critical factor in HPLC/UPLC method development. | Specified chemistry (C8, C18), particle size, dimensions, and lot-to-lot consistency. |
| Buffer Salts & Reagents | Used to create the mobile phase; factors like pH and ionic strength are often studied. | HPLC-grade; low UV absorbance; prepared with high-purity water. |
| Automated Liquid Handler (e.g., dragonfly discovery) | Enables high-precision, low-volume dispensing for setting up complex DoE assays, reducing human error and ensuring reproducibility [39]. | Non-contact dispensing; liquid agnostic; high accuracy at low volumes. |
| DoE Software (e.g., JMP, Stat-Ease, Minitab) | Used to generate optimal design matrices and perform statistical analysis of the results. | Support for D-, G-, and other optimality criteria; user-friendly interface. |
The strategic application of Design of Experiments provides a powerful pathway to efficient and reliable optimization in pharmaceutical method validation. By moving beyond OFAT and adopting a structured, multi-factorial approach, researchers can achieve a deeper level of process understanding, identify robust method conditions, and effectively control variation. The comparative data and protocols presented in this guide demonstrate that the strategic selection of a DoE criterion—be it D-optimal for screening or G-optimal for robustness—is crucial to meeting specific validation objectives. As the industry continues to evolve under QbD and ICH Q14 frameworks, embracing these advanced statistical tools is no longer optional but essential for any organization aiming to accelerate development, ensure regulatory compliance, and deliver high-quality pharmaceuticals to patients.
Ultra-High-Performance Liquid Chromatography (UHPLC) coupled with various mass spectrometric detectors, including High-Resolution Mass Spectrometry (HRMS) and tandem mass spectrometry (LC-MS/MS), represents a cornerstone of modern analytical chemistry. These advanced instrumental configurations provide the sensitivity, selectivity, and throughput required for challenging applications across pharmaceutical, environmental, and food safety domains [41]. The fundamental advancement of UHPLC over traditional HPLC lies in its operation at significantly higher pressures (typically up to 15,000 psi or greater), utilizing columns packed with sub-2-μm particles to achieve superior chromatographic resolution, decreased analysis time, and enhanced sensitivity [42] [43]. When these separation capabilities are coupled with the detection power of mass spectrometry, analysts gain a powerful toolkit for addressing complex analytical problems.
The selection of an appropriate mass spectrometric detector is crucial and depends heavily on the specific analytical requirements. HRMS instruments, such as Time-of-Flight (TOF) and Orbitrap analyzers, provide exact mass measurements with uncertainties in the fifth decimal place, enabling confident elemental composition assignment and non-targeted analysis [44]. In contrast, triple quadrupole (QqQ) mass spectrometers operating in LC-MS/MS mode offer exceptional sensitivity and specificity for targeted quantification through Selected Reaction Monitoring (SRM) or Multiple Reaction Monitoring (MRM) transitions [45] [41]. This guide provides a comprehensive comparison of these technologies, supported by experimental data and detailed methodologies, to assist researchers in selecting the optimal approach for their specific method validation requirements.
The core distinction between mass spectrometry platforms lies in their resolution and mass accuracy capabilities. Low-resolution mass spectrometers (like single quadrupoles) provide nominal mass measurements with uncertainties to the first decimal place, whereas high-resolution mass spectrometers provide exact mass measurements with uncertainties in the fifth decimal place [44]. This fundamental difference in mass accuracy directly impacts compound identification confidence and analytical workflow possibilities.
Table 1: Key Characteristics of Mass Spectrometry Platforms Coupled with UHPLC
| Platform | Mass Accuracy | Resolving Power | Primary Analysis Mode | Typential Applications |
|---|---|---|---|---|
| UHPLC-QqQ-MS/MS | Nominal mass (first decimal place) | Unit resolution (Low Resolution) | Targeted (e.g., MRM) | High-sensitivity quantification of known compounds [45] [41] |
| UHPLC-TOF-HRMS | High (≤5 ppm) | >10,000 FWHM [45] | Non-targeted/Targeted | Metabolomics, contaminant screening, metabolite identification [45] [44] |
| UHPLC-Orbitrap-HRMS | Very High (≤1-5 ppm) | Up to 120,000-240,000 FWHM [43] | Non-targeted/Targeted | Structural elucidation, retrospective analysis, complex matrix analysis [45] [46] |
The practical advantages of UHPLC-MS, regardless of the detector, include improved chromatographic resolution, reduced ion suppression from matrix components due to better separation, lower solvent consumption, and increased sample throughput [41]. However, these systems also present challenges, including frictional heating effects, requirements for high-quality solvents to prevent column blockage, and the need for rapid data acquisition to properly define narrow chromatographic peaks [41] [42].
Comparative Experimental Data and Performance Metrics
Direct comparisons between these platforms reveal their relative strengths and weaknesses in specific application scenarios. The following data, drawn from validation studies, highlights how instrument selection impacts key performance metrics.
Analysis of Hexabromocyclododecane (HBCD) Diastereomers
A rigorous comparative study evaluated UHPLC-TOF-HRMS, UHPLC-Orbitrap-HRMS, and UHPLC-QqQ-MS/MS for determining HBCD diastereomers in fish samples [45].
Table 2: Performance Comparison for HBCD Diastereomer Analysis in Fish [45]
| Performance Metric | UHPLC-TOF-HRMS | UHPLC-Orbitrap-HRMS | UHPLC-QqQ-MS/MS |
|---|---|---|---|
| Instrumental LOQ | 0.9 - 4.5 pg on-column | Data not specified in extract | Typically lower than HRMS |
| Method LOQ | 7.0 - 29.0 pg/g wet weight | Data not specified in extract | Data not specified in extract |
| Recovery (%) | 99 - 116 | Data not specified in extract | Data not specified in extract |
| Repeatability (RSD%) | 2.3 - 7.1 | Data not specified in extract | Data not specified in extract |
| Intermediate Precision (RSD%) | 2.9 - 8.1 | Data not specified in extract | Data not specified in extract |
| Key Finding | Performance suitable for trace analysis; response more affected by matrix components vs. other systems | Robust against matrix effects | Produced adequate and similar results to HRMS platforms |
A critical finding was that the analytical response of the UHPLC-TOF-HRMS system was more significantly affected by matrix components in the final extracts compared to the UHPLC-Orbitrap-HRMS and UHPLC-QqQ-MS/MS systems [45]. Despite this, all three techniques produced statistically similar results for the HBCD content in real fish samples, demonstrating that UHPLC-TOF-HRMS is an appropriate technique for this application when properly optimized [45].
Quantitative Analysis in Food and Biological Matrices
Other studies have further solidified the performance benchmarks for these technologies in regulated applications.
Table 3: Performance Data from Various Application Studies
| Application / Analytic | Platform | Reported Performance | Source |
|---|---|---|---|
| 17 Phytocannabinoids in plants, resins, oils | UHPLC-HRMS/MS (Orbitrap) | LOQ: 0.25-1.0 mg/kgRecovery: 95-100%Repeatability (RSD): 2-12% | [47] |
| Mycotoxins in grains and nuts | UHPLC-HRMS (Orbitrap) | Quantitative results "just as sensitive as the LC-MS/MS method" with more identification information | [46] |
| Pesticides in fruits and vegetables | UHPLC-HRMS (Orbitrap) | Method successfully validated; effective for screening large volumes of compounds | [46] |
| Veterinary Drugs in milk | UHPLC-HRMS (Orbitrap) | Method successfully validated | [46] |
A key advantage of HRMS noted in food safety analysis is its utility in large-scale screening. While LC-MS/MS is the established standard for targeted analysis of known contaminants, maintaining a method for hundreds of pesticides requiring multiple MRM transitions per compound is difficult. HRMS workflows, with HRMS/MS libraries and accurate mass databases, can screen for large numbers of chemical residues more manageably [46].
Experimental Protocols and Methodologies
Robust method development is fundamental for achieving reliable data. The following section outlines detailed experimental protocols cited in the comparative studies.
Sample Preparation Protocols
Effective sample preparation is critical to minimize matrix effects and ion suppression, particularly in complex biological samples [42].
- Cannabis Plants for Phytocannabinoid Analysis: A representative 0.5 g sample is weighed and extracted with 20 mL of ethanol on a laboratory shaker (240 RPM) for 30 minutes. After centrifugation (10,000 RPM, 5 min), the supernatant is collected, and the extraction is repeated. The combined extracts are brought to a final volume of 50 mL with ethanol [47].
- Resinous Matrices: A 50 mg sample is dissolved directly in 25 mL of ethanol using ultrasonication for 5 minutes [47].
- Matrices with High Oil Content: A 0.50 g sample is dissolved in 25 mL of ethanol using ultrasonication for 5 minutes [47].
- Fish Tissue for Antibiotic Analysis (QuEChERS): A common approach for multiresidue analysis is the QuEChERS (Quick, Easy, Cheap, Effective, Rugged, and Safe) method. This typically involves an acetonitrile extraction followed by a dispersive solid-phase extraction (d-SPE) clean-up step to remove fatty acids and other interferences [41] [46] [44].
UHPLC-HRMS Method for Phytocannabinoids
The following validated method provides a template for the simultaneous determination of 17 phytocannabinoids [47].
Chromatography:
- System: UHPLC (e.g., Thermo Scientific UltiMate 3000)
- Column: Acquity UPLC BEH C18 (100 x 2.1 mm, 1.7 μm)
- Mobile Phase A: Water-Methanol (95:5, v/v) with 5 mM Ammonium Formate and 0.1% Formic Acid
- Mobile Phase B: Isopropanol-Methanol-Water (65:30:5, v/v/v) with 5 mM Ammonium Formate and 0.1% Formic Acid
- Gradient: 5% B to 60% B in 1 min, to 70% B in 10 min, to 100% B in 0.5 min, hold 5 min.
- Flow Rate: 0.3 mL/min, increased to 0.4 mL/min during column wash
- Injection Volume: 3 μL
- Total Run Time: 19 minutes [47]
Mass Spectrometry (HRMS/MS):
- System: Q-Exactive Plus Orbital Trap Mass Spectrometer
- Ionization: Electrospray Ionization (ESI), positive/negative switching
- Full Scan MS Parameters: Resolution 70,000 FWHM, scan range 200-1000 m/z
- MS/MS (Parallel Reaction Monitoring - PRM): Resolution 17,500 FWHM, normalized collision energies (NCE) 28, 35, 42%
- Data Acquisition: Full scan MS followed by PRM for targeted quantification [47]
UHPLC-Orbitrap Method for Antibiotics in Fish
This method exemplifies a targeted/non-targeted approach for monitoring antibiotics and their unknown breakdown products [44].
Chromatography:
- System: Thermo Ultimate 3000 UHPLC
- Column: Hypersil GOLD (150 x 2.1 mm, 3 μm)
- Column Temperature: 40 °C
- Mobile Phase A: Water with 0.15% Formic Acid
- Mobile Phase B: Methanol
- Gradient: 25% B (hold 1 min), to 90% B (1-5 min), hold 90% B (5-8 min), re-equilibration.
- Flow Rate: 0.3 mL/min
- Total Run Time: 14 minutes [44]
Mass Spectrometry:
- System: Thermo Q-Exactive Quadrupole-Orbitrap
- Ionization: Electrospray Ionization, positive mode
- Acquisition Modes: Full-scan MS (for non-targeted screening) and parallel reaction monitoring (PRM, for targeted quantification)
- Accurate Mass Calibration: Internal mass calibration using a reference standard introduced via a secondary pump for sustained mass accuracy [44]
Workflow Visualization and Decision Pathways
The choice between LC-MS/MS and LC-HRMS is driven by the analytical scope. The following workflow diagram outlines a logical decision path for method selection.
Figure 1. Decision workflow for selecting between UHPLC-MS platforms. This pathway helps determine the most suitable instrumentation based on the analytical objectives, whether for targeted quantification with high sensitivity or for broader screening and identification workflows.
Essential Research Reagent Solutions
The reliability of UHPLC-MS analyses depends on the quality of reagents and consumables. The following table details key materials required for robust method execution.
Table 4: Essential Research Reagents and Materials for UHPLC-MS Analysis
| Reagent/Material | Function/Purpose | Technical Considerations |
|---|---|---|
| LC-MS Grade Solvents (Water, Methanol, Acetonitrile, Isopropanol) | Mobile phase components; sample reconstitution | Minimizes background noise and system contamination; essential for stable baselines and high sensitivity [47]. |
| Ammonium Formate / Formic Acid | Mobile phase additives for pH control and ionization | Promotes protonation/deprotonation in ESI; volatile and MS-compatible. Concentration typically 2-10 mM and 0.1% respectively [47]. |
| Stable Isotope-Labeled Internal Standards (SIL-IS) | Normalization for quantification | Corrects for matrix effects and recovery losses during sample preparation; most reliable approach for precise bioanalysis [42]. |
| High-Purity Analytical Standards | Calibration and compound identification | Used for instrument calibration, preparation of quality control (QC) samples, and MS/MS spectral library generation [47] [46]. |
| Sub-2 μm UHPLC Columns (e.g., C18) | Chromatographic separation | Provides high-resolution separation of complex mixtures; core component of UHPLC systems [47] [42]. |
| Mass Calibration Solutions | Instrument mass accuracy calibration | Pre-mixed reference standards for external and internal mass calibration of HRMS instruments, ensuring sub-ppm mass accuracy [44]. |
UHPLC, HRMS, and LC-MS/MS represent a suite of powerful, complementary technologies that serve distinct yet sometimes overlapping roles in the modern analytical laboratory. UHPLC-QqQ-MS/MS remains the gold standard for targeted, high-sensitivity quantification of known analytes, as evidenced by its widespread use in routine monitoring and regulated methods [41] [46]. Conversely, UHPLC-HRMS platforms (Orbitrap and TOF) provide unparalleled capabilities for non-targeted screening, structural elucidation, and retrospective data analysis, making them ideal for discovery metabolomics, contaminant identification, and method development [45] [44].
The choice between these platforms is not a matter of superiority but of strategic alignment with analytical goals. For projects requiring the ultimate sensitivity for a defined set of targets, QqQ systems are optimal. When the analytical scope is broader, less defined, or requires high confidence in compound identification, HRMS is the clear choice. As the technology continues to evolve, the integration of these platforms and the development of hybrid workflows will further empower researchers in drug development and related fields to meet the growing demands of complex sample analysis with precision, accuracy, and efficiency.
In pharmaceutical development and manufacturing, the reliability of analytical methods is not a single event but a process that spans the entire lifespan of a product. This process, known as method lifecycle management, systematically ensures that methods remain fit-for-purpose from initial validation through routine commercial use. For researchers and drug development professionals, implementing a robust lifecycle approach is fundamental to generating reliable, reproducible data that meets regulatory standards.
The core of this lifecycle comprises three distinct but interconnected stages: validation, monitoring, and verification. Validation establishes through laboratory studies that the performance characteristics of a method meet requirements for its intended analytical applications [1]. Monitoring constitutes the ongoing, planned sequence of observations or measurements to ensure a process remains in control [48]. Verification serves as the periodic confirmation that the method continues to perform as effectively as when it was first validated [49]. Understanding the purpose, timing, and requirements of each stage is critical for maintaining data integrity and regulatory compliance throughout a product's commercial life.
Core Concepts: Validation, Monitoring, and Verification
Although often used interchangeably, validation, monitoring, and verification represent distinct activities within the quality management process, each with a specific role at different points in the method lifecycle [48]. The relationship between these elements forms the foundation of effective lifecycle management.
Validation is about obtaining evidence that a control measure or combination of control measures can effectively control a significant hazard [48]. In analytical terms, it is the process of establishing, through laboratory studies, that the performance characteristics of a method meet the requirements for its intended analytical applications [1]. It answers the question: "Can this method work?" and is performed before a method is put into routine use, when it is first designed, or when significant changes are made [48].
Monitoring involves determining the status of a system, process, or activity through a planned sequence of observations or measurements [48]. Its primary goal is to provide information for timely action, enabling the detection of deviations from established critical limits and allowing for immediate corrective actions [48]. It is an activity performed during an operational process, often very frequently—sometimes as often as every hour or at the start and end of every production shift [50].
Verification is the confirmation, through the provision of objective evidence, that specified requirements have been fulfilled [48]. It answers the question: "Is the method still working as expected?" [50]. This is a periodic activity applied after a method has been in use, typically at regular annual intervals, to confirm that the process continues to be as effective as when it was first validated [48] [49].
The following workflow illustrates how these three concepts interact throughout the method lifecycle:
Analytical Performance Parameters in Method Validation
Method validation typically evaluates a standard set of analytical performance characteristics to demonstrate the method is suitable for its intended use. The United States Pharmacopeia (USP) outlines key validation characteristics, including Accuracy, Precision, Specificity, and others [1]. The evaluation of these parameters provides the experimental foundation for proving method reliability.
- Accuracy refers to the closeness of test results obtained by the method to the true value. It is typically determined by measuring the recovery of a known, spiked amount of analyte or by comparing results to a reference method [1].
- Precision expresses the degree of agreement among individual test results when the method is applied repeatedly to multiple samplings of a homogeneous sample. It is usually investigated at repeatability (same day, same analyst) and intermediate precision (different days, different analysts) levels [1].
- Specificity is the ability of the method to assess the analyte unequivocally in the presence of other components that may be expected to be present, such as impurities, degradation products, or matrix components [1].
- Linearity and Range: Linearity is the method's ability to generate results that are directly proportional to the analyte concentration. The range is the interval between the upper and lower concentration levels for which suitable levels of precision, accuracy, and linearity have been demonstrated [1].
- Robustness measures the method's capacity to remain unaffected by small, deliberate variations in procedural parameters, such as temperature, pH, or mobile phase composition, and provides an indication of its reliability during normal usage [1].
Experimental Protocols for Key Validation Parameters
Protocol for Assessing Accuracy and Precision:
- Sample Preparation: Prepare a minimum of five replicates of a quality control (QC) sample at three different concentration levels (low, medium, and high) covering the validated range.
- Analysis: Analyze all QC samples in a single batch (for repeatability) or over multiple days by different analysts (for intermediate precision).
- Calculation:
- Accuracy: Calculate the mean percent recovery for each concentration level and the overall mean.
% Recovery = (Mean Observed Concentration / Nominal Concentration) * 100. - Precision: Calculate the relative standard deviation (RSD) for the replicates at each concentration level.
RSD (%) = (Standard Deviation / Mean) * 100.
- Accuracy: Calculate the mean percent recovery for each concentration level and the overall mean.
- Acceptance Criteria: For a typical chromatographic assay, accuracy might be required to be within 98.0-102.0% recovery, and precision (RSD) should be ≤2.0%.
Protocol for Specificity/Selectivity:
- Interference Check: Analyze the sample matrix (placebo) without the analyte.
- Forced Degradation: Analyze samples of the drug substance or product that have been subjected to stress conditions (e.g., acid/base hydrolysis, oxidation, thermal degradation, photolysis).
- Data Interpretation: The chromatograms are examined to ensure the analyte peak is pure and free from interference from other peaks, confirming the method's ability to quantify the analyte accurately.
Comparative Analysis of Lifecycle Stages
The table below provides a structured comparison of the three core lifecycle stages, highlighting their distinct purposes, timing, and key activities.
Table 1: Comparative Analysis of Validation, Monitoring, and Verification
| Aspect | Validation | Monitoring | Verification |
|---|---|---|---|
| Core Question | "Can the method work for its intended purpose?" [1] | "Is the process in control right now?" [48] | "Does the method still perform as originally validated?" [49] |
| Primary Goal | To establish performance characteristics for the intended application [1] | To enable timely detection of deviations for corrective action [48] | To provide objective evidence of continued conformity [48] |
| Timing/Frequency | Before routine use; at method design or after significant changes [48] | During operation; frequently (e.g., start/end of shift, every batch) [50] | After operation; periodically (e.g., annually) [49] [50] |
| Key Activities | - Accuracy & Precision studies- Specificity & Linearity assessment- Determination of Range & Robustness [1] | - Planned sequence of observations/measurements [48]- Running control samples/test pieces [50]- Checking device settings | - Comprehensive performance review [50]- Comparative testing against original validation data [49]- Personnel training review |
| Typical Output | Formal validation report with objective evidence and data [49] | Real-time data logs, control charts, and records of any deviations [50] | Verification report documenting continued compliance with specifications [50] |
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful execution of method validation, monitoring, and verification relies on a set of essential materials and reagents. The following table details key items and their functions in the analytical lifecycle.
Table 2: Key Reagent Solutions for Analytical Lifecycle Management
| Tool/Reagent | Function in Lifecycle Management |
|---|---|
| Certified Reference Standards | Provides a characterized substance with a defined purity, serving as the benchmark for quantifying the analyte and establishing method accuracy during validation and verification [1]. |
| System Suitability Test (SST) Mixtures | A prepared mixture of analytes and/or impurities used to confirm that the analytical system (e.g., HPLC) is performing adequately before and during a sequence of analyses, crucial for both monitoring and verification. |
| Quality Control (QC) Samples | Samples with known or accepted concentrations of the analyte, used to continuously monitor the method's performance over time (precision and accuracy) during routine analysis. |
| Forced Degradation Samples | Samples intentionally degraded under various stress conditions; used during validation to demonstrate the method's specificity and stability-indicating properties [1]. |
| Stable Isotope-Labeled Internal Standards | Used in mass spectrometric methods to correct for analyte loss during sample preparation and for matrix effects, significantly improving the precision and accuracy of the measurement. |
A systematic approach to method lifecycle management, from rigorous initial validation through to diligent routine monitoring and periodic verification, is non-negotiable in modern drug development. This structured framework is not merely a regulatory hurdle but a fundamental scientific practice that ensures the generation of reliable, high-quality data. For researchers and scientists, mastering the distinctions and linkages between these stages is key to maintaining method integrity, ensuring product quality, and safeguarding patient safety throughout a product's lifecycle. As regulatory landscapes evolve, a proactive and well-documented lifecycle strategy remains the best defense against method failure and its associated risks.
Navigating Challenges: Troubleshooting and Optimizing Method Performance
Identifying and Mitigating Common Pitfalls in Method Validation
Method validation serves as the foundational process for proving that an analytical procedure consistently produces reliable, accurate, and reproducible results suitable for its intended purpose [51]. In regulated environments such as pharmaceutical development and clinical testing, method validation acts as a critical gatekeeper of quality, safeguarding product integrity and patient safety [51]. Regulatory frameworks including FDA Analytical Procedures and Methods Validation, ICH Q2(R1), and USP <1225> mandate rigorous validation, with non-compliance risking costly delays, regulatory rejections, or product recalls [51] [52]. Despite this recognized importance, laboratories frequently encounter recurring pitfalls that compromise data integrity, regulatory compliance, and operational efficiency. This guide systematically identifies these common challenges, provides comparative analysis of validation approaches, and offers evidence-based mitigation strategies supported by experimental data and practical protocols.
Common Pitfalls in Method Validation: Identification and Impact
Analytical laboratories, particularly those operating across multiple regulatory jurisdictions, face recurring challenges that can undermine method validity. The table below summarizes the most prevalent pitfalls, their consequences, and frequency across different laboratory types.
Table 1: Common Method Validation Pitfalls and Their Organizational Impact
| Pitfall Category | Specific Manifestations | Potential Consequences | Prevalence in Regulatory Audits |
|---|---|---|---|
| Inadequate Specificity | Failure to test across all relevant matrices; insufficient interference testing [51] | Inaccurate quantification of analyte; false positive/negative results [51] | High (FDA, EMA) |
| Precision & Accuracy Gaps | Too few replicates; improper spike recovery studies; ignoring matrix effects [51] [52] | Reduced method reliability; unacceptable %RSD; biased results [3] | Very High (All agencies) |
| Incomplete Linearity & Range | Insufficient calibration points; range not covering expected concentrations [51] [5] | Inaccurate quantification at concentration extremes [5] | Moderate-High |
| Poor Robustness Testing | Failure to test method under deliberate variations [51] [53] | Method failure during routine use; transfer failures [53] | Moderate |
| Documentation Deficiencies | Missing data or protocol gaps; inadequate change control [51] [53] | Regulatory citations; audit failures; inability to trace decisions [51] | High |
The interconnected nature of these pitfalls means that weaknesses in one parameter often cascade into other areas. For instance, inadequate specificity testing can undermine accuracy claims, while poor documentation obscures these fundamental flaws during internal review processes [51]. Regulatory agencies including the FDA and EMA specifically focus on these areas during inspections, with precision, accuracy, and specificity representing the most frequently cited deficiencies in laboratory audits [51] [52].
Comparative Analysis of Validation Parameters Across Techniques
The performance of analytical methods varies significantly across different instrumental techniques, with each presenting unique vulnerability profiles. Understanding these technique-specific considerations is essential for effective risk mitigation.
Table 2: Technique-Specific Validation Risks and Acceptance Criteria
| Analytical Technique | Highest Risk Parameters | Recommended Acceptance Criteria | Comparative Performance Data |
|---|---|---|---|
| HPLC/LC-MS | Precision (retention time shifts), Specificity (peak interference) [51] | %RSD ≤2% for precision; resolution ≥1.5 between critical pairs [53] | LC-MS shows 30-50% better sensitivity but similar precision challenges vs. HPLC |
| GC | Precision (temperature sensitivity), Carryover [51] | %RSD ≤2%; carryover ≤0.5% [54] | GC demonstrates higher temperature sensitivity than HPLC methods |
| UV-Vis Spectroscopy | Accuracy (baseline drift), Linearity [51] | r² ≥ 0.99; 95-105% recovery for accuracy [53] [5] | Wider linear range but greater matrix interference potential vs. chromatographic methods |
| Immunoassays | Specificity (cross-reactivity), LOQ [52] | Cross-reactivity <5% for similar compounds [52] | Higher throughput but reduced specificity compared to chromatographic techniques |
The data reveals that while chromatographic methods (HPLC, GC) generally offer superior specificity and precision, they present greater operational complexity and sensitivity to parameter variations [51]. Spectroscopic techniques like UV-Vis provide broader linear ranges but demonstrate higher susceptibility to matrix effects that compromise accuracy [51]. Techniques handling biological samples (e.g., LC-MS/MS for bioanalytical work) require additional validation for matrix effects and incurred sample reanalysis [52].
Experimental Protocols for Key Validation Parameters
Accuracy and Precision Assessment
Protocol for Accuracy Determination via Spike Recovery:
- Prepare a blank matrix sample (devoid of analyte) and fortify with known concentrations of analyte standard at 80%, 100%, and 120% of target concentration [3] [53]
- Analyze fortified samples using the method under validation (n=6 per concentration level)
- Calculate percent recovery: (Measured Concentration/Theoretical Concentration) × 100
- Acceptance criterion: Mean recovery of 95-105% with %RSD ≤2% for precision [53]
Protocol for Precision Evaluation:
- Analyze six independent preparations of homogeneous sample at 100% target concentration
- Conduct repeatability studies (same analyst, same day) and intermediate precision (different days, analysts, or instruments) [53]
- Calculate mean, standard deviation, and %RSD for measured concentrations
- Compare obtained %RSD against modified Horwitz criteria: %RSDr ≤ 2.1% for 5% analyte concentration [5]
Specificity and Selectivity Testing
Protocol for Chromatographic Methods:
- Inject chromatographic blanks (matrix without analyte) to confirm absence of interfering peaks at analyte retention time [5]
- Analyze samples containing likely interferents (degradation products, matrix components, related compounds)
- Verify peak purity using diode array detection or mass spectrometry
- Resolution between analyte and closest eluting potential interferent should be ≥1.5 [53]
Linearity and Range Establishment
Protocol for Linearity Assessment:
- Prepare standard solutions at minimum five concentrations spanning 50-150% of expected working range [5]
- Analyze each concentration in duplicate or triplicate
- Plot mean response against concentration and perform linear regression
- Calculate correlation coefficient (r² ≥ 0.99), y-intercept, and slope [53] [5]
- Verify relative standard deviation of response factors ≤2%
Visualization of Method Validation Relationships and Workflows
Figure 1: Method Validation Workflow showing the three critical phases from planning through documentation, with key activities at each stage.
Advanced Mitigation Strategies for Seasoned Professionals
Quality by Design (QbD) Principles
Implementing QbD during method development creates more robust validation outcomes [51] [52]. This systematic approach involves:
- Identifying critical method parameters (e.g., mobile phase pH, column temperature, gradient profile) [52]
- Determining method operable design region (MODR) through design of experiments (DoE) [53]
- Establishing control strategies for parameters within the MODR
- Implementing statistical process control (SPC) charts for ongoing performance verification [53]
Design of Experiments (DoE) Applications
Rather than one-factor-at-a-time testing, DoE efficiently explores multiple variables and their interactions [53]. For robustness testing:
- Identify critical factors (pH, temperature, flow rate, etc.)
- Design fractional factorial or response surface methodology experiments
- Model factor effects on critical quality attributes (precision, accuracy, resolution)
- Establish permissible ranges for each factor to maintain method performance
Lifecycle Management and Revalidation
A validated method requires ongoing monitoring and management [53]:
- Implement periodic review (annually or following major instrument changes)
- Establish change control procedures with predefined revalidation thresholds
- Maintain system suitability test (SST) tracking with control charts
- Document all method changes and performance trends
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Validation Experiments
| Reagent/Material | Specific Function in Validation | Quality Requirements | Application Examples |
|---|---|---|---|
| Certified Reference Standards | Accuracy determination; calibration curve establishment [3] | Certified purity with uncertainty statement; traceable documentation | Quantification of active ingredients; method calibration [3] |
| Matrix-Matched Materials | Specificity testing; accuracy assessment [51] | Well-characterized composition; representative of actual samples | Selectivity verification in biological samples [52] |
| System Suitability Test Mixtures | Daily method performance verification [53] | Stable composition; containing critical analytes | HPLC column performance monitoring [53] |
| Stability Samples | Forced degradation studies; stability-indicating method validation [51] | Controlled degradation conditions; well-documented treatment | Specificity demonstration for impurity methods |
Effective method validation requires meticulous attention to common pitfalls throughout the method lifecycle. The comparative data presented demonstrates that technique-specific vulnerabilities demand tailored validation approaches, while fundamental parameters like specificity, accuracy, and precision remain universally critical. By implementing the experimental protocols, advanced statistical approaches, and systematic workflows outlined in this guide, laboratories can significantly enhance method reliability, regulatory compliance, and data integrity. The evolving regulatory landscape continues to emphasize lifecycle management approaches, making continuous method verification and improvement essential components of sustainable quality systems in analytical science.
Managing Analytical Complexity in Novel Modalities (Cell and Gene Therapies)
Analytical Landscape of Advanced Therapy Modalities
The field of cell and gene therapies (CGTs) represents a frontier in modern medicine, characterized by its rapid scientific evolution and unique analytical challenges. Since the first CAR T-cell therapies entered the market in 2017, the landscape has expanded to include treatments for sickle cell disease, hemophilia, and solid tumors, utilizing diverse platforms including gene editing and tumor-infiltrating lymphocyte (TIL) technologies [55]. By 2025, there are more than 22 FDA-approved therapies on the market with projections forecasting over 200 approvals and 100,000 treated patients in the US by 2030 [55].
This growth introduces significant complexity in analytical method development and validation. Unlike traditional pharmaceuticals, cell and gene therapies are often personalized medicines with individualized manufacturing processes, creating inherent variability that challenges conventional analytical approaches [55] [56]. The industry faces persistent hurdles in chemistry, manufacturing, and controls (CMC) requirements throughout therapy development and commercialization [55]. Furthermore, these therapies present stringent handling and storage requirements and complex reimbursement models that further complicate their analytical characterization and standardization [55].
Comparative Analysis of Therapeutic Modalities
Key Modalities and Technical Specifications
Table 1: Comparative Analysis of Advanced Therapy Modalities
| Modality | Technical Complexity | Manufacturing Scale | Key Analytical Challenges | 2025 Market Position |
|---|---|---|---|---|
| Cell Therapies | High | Primarily autologous | Scalable logistics, manufacturing hurdles, successful commercialization [57] | Proven potential with process refinement pending [57] |
| AAV Gene Therapies | High | Commercial scale emerging | Immunogenicity, indication selection, scalable production [57] | Rising from reset with key 2024 approvals [57] |
| mRNA Technologies | Medium-high | Scalable | Targeted in vivo delivery, finding optimal applications [57] | Reassessment phase post-pandemic [57] |
| Oligonucleotides | Medium | Scalable | Commercial pathway establishment beyond rare diseases [57] | Breakthrough year in 2024 with continued growth expected [57] |
Performance Metrics Across Modalities
Table 2: Quantitative Performance Metrics for Advanced Therapies
| Performance Metric | Cell Therapies | AAV Gene Therapies | mRNA Platforms | Oligonucleotides |
|---|---|---|---|---|
| Approval Count (2025) | Multiple (Amtagvi, Tecelra, Aucatzyl) [57] | 3+ (BEQVEZ, KEBILIDI, Elevidys) [57] | 1 (mRESVIA) [57] | Multiple (Olezarsen, Rivfloza) [57] |
| Manufacturing Timeline | Weeks (patient-specific) [55] | Commercial scale [57] | Rapid production [57] | Commercial scale [57] |
| Durability Data | Varies; long-term follow-up required [55] | 5-year data emerging [56] | Under investigation [57] | Established long-term data [57] |
| Physician Experience | Increasing (avg. 25 patients/oncologist) [56] | Growing with expanded approvals [57] | Limited to specific applications [57] | Established and growing [57] |
Method Validation Frameworks
Validation Versus Verification Protocols
In regulated product testing, understanding method validation versus verification is fundamental. Method validation is defined as a process through laboratory studies that establishes the performance characteristics of a method meet requirements for its intended analytical applications [1]. For compendial methods (e.g., USP, BP, EP), method verification is required to determine suitability under actual conditions of use [1].
Table 3: Method Validation Parameters and Specifications
| Validation Parameter | Definition | Acceptance Criteria Framework |
|---|---|---|
| Accuracy | Closeness of test results to true value [1] | Must be determined across method's range [1] |
| Precision | Degree of agreement among repeated measurements [1] | Multiple samplings of homogeneous sample [1] |
| Specificity | Ability to assess analyte unequivocally [1] | In presence of impurities, degradation products, matrix interferences [1] |
| Detection Limit | Lowest amount detectable [1] | For limit tests [1] |
| Quantitation Limit | Lowest amount quantifiable [1] | With acceptable precision and accuracy [1] |
| Linearity | Ability to obtain proportional results [1] | Directly proportional to analyte concentration [1] |
| Range | Interval between upper/lower analyte levels [1] | Yielding suitable precision, accuracy, linearity [1] |
| Robustness | Capacity to remain unaffected [1] | By small, deliberate procedural variations [1] |
Experimental Protocol: Potency Assay Validation
Objective: Establish validated potency assay for chimeric antigen receptor (CAR) T-cell therapy.
Materials:
- CAR T-cell product
- Target antigen-positive and negative cell lines
- Flow cytometer with appropriate detectors
- Cytokine detection ELISA kit
- Cell culture reagents and equipment
Methodology:
- CAR Expression Quantification:
- Stain CAR T-cells with anti-CAR detection antibody
- Analyze by flow cytometry using fluorescence quantification beads
- Calculate CAR molecules per cell
Target Cell Killing:
- Co-culture CAR T-cells with target cells at multiple effector:target ratios (e.g., 1:1, 5:1, 10:1)
- Measure target cell viability after 24-48 hours using validated viability stains
- Calculate percentage specific lysis
Cytokine Secretion:
- Collect supernatant from co-cultures after 24 hours
- Measure IFN-γ and IL-2 by ELISA
- Compare to unstimulated CAR T-cell controls
Data Analysis:
- Establish dose-response curves for target cell killing
- Determine correlation between CAR expression and functional activity
- Calculate assay precision (CV < 20%) and accuracy (80-120% recovery)
Figure 1: Potency Assay Validation Workflow
Essential Research Reagent Solutions
Table 4: Key Research Reagents for Cell and Gene Therapy Analytics
| Reagent Category | Specific Examples | Function in Analytical Development |
|---|---|---|
| Vector Standards | AAV reference standards, Lentiviral titer standards [57] | Quantification and quality control of gene delivery vehicles [57] |
| Cell Characterization | CAR detection antibodies, Viability markers, Cell subset panels [55] | Identity, purity, and potency assessment of cellular products [55] |
| Molecular Assays | qPCR reagents for vector copy number, TRAC primers, Sequencing panels [57] | Genetic modification verification and safety assessment [57] |
| Cytokine Detection | Multiplex cytokine panels, ELISA kits, ELISpot reagents [55] | Functional potency and immune activation monitoring [55] |
| Process Analytics | Metabolite assays, Endotoxin detection, Mycoplasma testing [1] | Manufacturing process monitoring and safety testing [1] |
Implementation Challenges and Analytical Solutions
Navigating Technical Complexity
The implementation of robust analytical methods for cell and gene therapies faces several persistent challenges. Logistical coordination remains particularly complex, as delays in any part of the process from leukapheresis to post-manufacturing delivery can jeopardize treatment viability [55]. The individualized manufacturing processes create inherent variability that must be characterized and controlled through rigorous analytics [55]. Additionally, biomanufacturing demand continues to outpace supply, especially as oncology therapies expand into new indications [57].
Advanced analytical solutions are emerging to address these challenges. Innovations in vector design including AI-enabled vector design and CNS-targeting capsids are unlocking greater precision in tissue-specific targeting for AAV therapies [57]. Advancements in scalable manufacturing and high-yield producer cell lines are de-risking pipelines by streamlining production [57]. Furthermore, bioprocessing advancements are focusing particularly on QC/QA and filtration to better discriminate between empty, partial, and full capsids [57].
Figure 2: Challenges and Analytical Solutions
Validation in Commercial Transition
As cell and gene therapy products transition from clinical to commercial stages, analytical strategies must evolve accordingly. The BIOSECURE Act has introduced uncertainty in U.S.-China supply chain relationships, raising questions about long-term impacts on biomanufacturing and necessitating diversified sourcing of critical reagents [57]. Coverage inconsistencies and cost-sharing requirements continue to limit patient access, creating pressure to demonstrate analytical consistency across product batches [55]. The field is also seeing a shift toward earlier lines of therapy, requiring more sensitive analytical methods to detect subtle product differences that may impact efficacy [56].
The 2025 landscape shows promising developments with increased oncologist familiarity with cell and gene therapies (average patients treated rising from 17 to 25 annually) driving more sophisticated analytical questions [56]. The expansion into autoimmune diseases and larger therapeutic areas like diabetes and cardiovascular disease necessitates adaptation of analytical methods developed for rare diseases to more common conditions [56]. Furthermore, real-world evidence systems are being leveraged for long-term follow-up, requiring analytical methods that can generate data comparable across multiple sites and over extended periods [55].
Overcoming Data Overload with AI and Centralized Data Platforms
In laboratories worldwide, scientific teams are generating more data than ever before. While this data holds enormous potential for innovation in drug development and scientific research, it often remains highly fragmented—created by different instruments, stored in disparate systems, and interpreted through different points of view [58]. This data overload forces scientists to spend countless hours searching for information that should be readily available, diverting valuable time from core research activities [58]. Within the critical context of method validation, precision, and accuracy verification research, this fragmentation introduces significant risk, potentially compromising data integrity, traceability, and ultimately, the reliability of scientific conclusions.
The evolution of centralized data platforms, now supercharged with Agentic AI, represents a paradigm shift in how research data is managed and utilized. These platforms are transforming data from a passive output into an active, contextualized asset that can be queried conversationally, much like consulting a domain-expert digital colleague [58]. This article provides a comparative analysis of how modern data platforms and AI technologies are not merely storing information, but are actively enabling researchers to overcome data overload while upholding the stringent demands of validation and verification science.
The Evolution: From Data Silos to Intelligent Data Fluency
The first wave of cloud-based solutions, often termed SaaS 1.0, addressed basic accessibility but failed to solve the core problem of data contextualization [58]. While data became easier to access and store, scientists were still left as data wranglers, navigating siloed systems and piecing together incomplete datasets—tasks that are not their core competency [58]. The inefficiencies stemming from this data overload don't just slow innovation; they introduce risk, lower reproducibility, and drain resources [58].
The next advancement, SaaS 2.0 or "Service-as-a-Software," enriches cloud platforms with Agentic AI [58]. This evolution moves beyond simple data access to genuine data fluency. The "service" in this model is the ability for lab workers to interact with intelligent agents in natural language. These AI agents respond to prompts, understand complex lab workflows, initiate tasks, and—most critically—surface contextualized data exactly when it's needed [58]. For validation research, where the pedigree of every data point is crucial, these embedded AI agents function as digital coworkers with extensive, domain-specific training grounded in verified lab and company data [58].
Table 1: Traditional vs. Modern AI-Powered Data Platforms
| Feature | Traditional SaaS (SaaS 1.0) | AI-Powered Service-as-a-Software (SaaS 2.0) |
|---|---|---|
| Core Philosophy | Cloud-delivered software for data access [58] | AI-driven services enabling conversation with data [58] |
| User Interaction | Manual software operation [58] | Natural language prompts to AI agents [58] |
| Intelligence & Automation | Limited, standardized automation [58] | Context-aware AI that understands scientific workflows [58] |
| Data Handling | Basic reporting and storage [58] | Predictive, domain-specific analytics [58] |
| Traceability | Manual provenance tracking | Built-in data pedigrees and governance via rigorous ontologies [58] |
Comparative Analysis of Leading AI Data Platforms
The market offers a diverse ecosystem of platforms designed to tackle data overload. The following comparison outlines key contenders, highlighting their distinct approaches to powering AI-driven research.
Table 2: Comparative Analysis of Leading AI and Data Platforms
| Platform | Primary Specialty | Key Features for Research & Validation | Considerations for Method Validation |
|---|---|---|---|
| Microsoft Intelligent Data Platform | Unified cloud data analytics | Integrates database management, analytics (Azure Synapse), visualization (Power BI), and compliance (Purview) [59]. | Strong for regulated environments; combines transaction processing with analytics, reducing time from data collection to analysis [59]. |
| Amazon Redshift | Cloud data warehousing | High-performance analysis via parallel processing, columnar storage. Features Redshift Serverless and zero-ETL integrations for real-time analytics [59]. | Deep integration with AWS AI services (SageMaker) can streamline model training and validation workflows on large datasets [59]. |
| Google BigQuery | Serverless, scalable data analytics | Separates storage and compute; processes petabytes rapidly. Incorporates machine learning for pattern identification and real-time analysis [59]. | Enables fast re-analysis of large historical datasets, which is useful for retrospective method validation and robustness checks. |
| Snowflake | Cloud-native data platform | Unique architecture separating storage, compute, and cloud services. Allows independent scaling and a marketplace for third-party data [59]. | Flexibility in managing data from multiple sites or CROs, which is common in collaborative drug development projects. |
| Databricks | Unified "Lakehouse" architecture | Combines data lake and warehouse functionality. Includes MLflow for experiment tracking and Delta Lake for data reliability [59]. | MLflow is critical for tracking machine learning experiments, ensuring reproducibility in AI-driven analytical model development [59]. |
| NVIDIA AI Enterprise Platform | Accelerated AI infrastructure | Hardware and software suite (Blackwell GPUs, BlueField DPUs, NeMo Retriever) optimized for AI data processing and RAG [60]. | Maximizes throughput for compute-intensive tasks like molecular simulation or analyzing high-dimensional data from complex assays. |
| Pinecone | Managed vector database | Specialized for high-speed storage and retrieval of vector embeddings, essential for semantic search and RAG applications [61]. | Ideal for finding similar experimental protocols or historical validation reports quickly via contextual search, not just keywords. |
| Cloudera | Enterprise big data analytics | Unified suite for data warehousing, machine learning, and streaming analytics across various industries [59]. | Provides a consolidated environment for managing the entire data lifecycle, from raw instrument data to analyzed results. |
Method Validation in the Age of AI: Precision, Accuracy, and Data Integrity
The principles of method validation—accuracy, precision, specificity, linearity, and robustness—are the bedrock of reliable scientific research, particularly in drug development [3] [5]. AI and centralized platforms do not replace these principles but provide powerful new tools to uphold them with greater efficiency and traceability.
Foundational Validation Parameters
- Accuracy refers to the closeness of agreement between a measured value and its true value. It is often determined through spike recovery experiments, where a known amount of analyte is added to the matrix and the percentage recovered is calculated [3] [5].
- Precision expresses the closeness of agreement between a series of measurements under the same conditions. It is measured as the standard deviation (SD) or relative standard deviation (%RSD) of multiple samplings [5]. The Horwitz equation provides an empirical model for expected precision, helping researchers gauge the acceptability of their method's repeatability [5].
- Linearity and Range demonstrate the method's ability to elicit results proportional to analyte concentration within a specified range [5]. This is established by analyzing a minimum of five concentrations and performing linear regression [5].
- Limit of Detection (LOD) and Limit of Quantification (LOQ) are mathematically derived from the linear calibration curve. LOD (typically a signal-to-noise ratio of 3:1) is the lowest detectable level, while LOQ (typically 10:1) is the lowest quantitatively measurable level with acceptable precision and accuracy [5].
The AI and Platform Advantage in Validation
Centralized platforms directly support validation research by ensuring data integrity and provenance. AI agents, when grounded in a semantic framework and rigorous data ontologies, can automatically tag data with its experimental context, track its lineage, and prevent the use of non-validated or out-of-specification data in critical analyses [58]. This built-in traceability is a safeguard against the "hallucinations" that can plague general AI models, as responses are tied to verified internal data [58].
Furthermore, AI can accelerate validation workflows. For instance, an AI agent can be queried: "Have we run stability tests on any compound similar to molecule 1234 in the past 6 months?" [58]. Instead of a scientist manually searching multiple systems, the AI instantly surfaces the relevant historical data, such as results for molecules 4514, 8515, and 145 [58]. This allows for rapid, data-driven decisions in method development based on a comprehensive view of all existing evidence.
Essential Research Toolkit for AI-Driven Data Management
The following reagents, software, and platforms constitute a modern toolkit for managing research data and implementing AI solutions in a scientific setting.
Table 3: The Scientist's AI and Data Management Toolkit
| Tool / Solution | Category | Primary Function in Research |
|---|---|---|
| Reference Standards | Research Reagent | High-purity materials with certificates of analysis used to calibrate instruments and methods, establishing accuracy and linearity [3]. |
| Certified Reference Materials (e.g., from NIST) | Research Reagent | Matrix-matched materials with known analyte concentrations and defined uncertainty, used for definitive accuracy determination and method validation [3]. |
| LabVantage (SaaS 2.0 Platform) | Informatics Platform | An AI-powered lab informatics platform that uses Agentic AI to transform data overload into data fluency via natural language queries [58]. |
| MLflow | Software Tool | An open-source platform for managing the complete machine learning lifecycle, including experiment tracking, model reproducibility, and deployment [59]. |
| NeMo Retriever | AI Software | A specialized tool for implementing high-performance Retrieval-Augmented Generation (RAG), grounding AI responses in proprietary enterprise data to ensure accuracy [60]. |
| TensorFlow / PyTorch | AI Framework | Open-source libraries for building and deploying custom machine learning models, such as predictive models for analytical outcomes or compound properties [62]. |
| Chromatographic Data Systems (CDS) | Informatics Software | Primary software for acquiring, processing, and managing data from chromatographic instruments, forming the core record for many analytical methods. |
Experimental Workflow: Integrating AI and Centralized Data in a Validation Study
The following diagram illustrates a modern, integrated workflow for an analytical method validation study, highlighting how AI and a centralized data platform interact with traditional wet-lab and analytical steps.
Diagram 1: AI-Integrated Validation Workflow. This workflow shows the seamless flow from physical experiments to AI-powered data analysis within a centralized platform, ensuring traceability and rapid insight generation.
Detailed Protocol for a Validation Experiment Leveraging an AI Platform
Experiment: Determination of Accuracy and Precision for a Novel Bioactive Compound Assay.
1. Hypothesis: The proposed HPLC-UV method can accurately and precisely quantify the target compound in a plasma matrix over a concentration range of 1-100 μg/mL.
2. Centralized Platform Setup:
- The experimental plan, including sample identifiers, target concentrations, and matrix details, is pre-registered in the centralized data platform (e.g., a next-generation LIMS like LabVantage) [58].
- The AI agent's semantic framework is configured with the relevant ontology for "accuracy," "precision," "plasma matrix," and "HPLC."
3. Sample Preparation & Data Acquisition:
- Prepare validation standards by spiking the analyte into blank plasma at concentrations of 1, 5, 10, 50, and 100 μg/mL (covering the range of 50-150% of the target) [5]. Each concentration is prepared and analyzed in quintuplicate (n=5) [5].
- Inject the standards into the HPLC system. The Chromatographic Data System (CDS) is integrated with the central platform, automatically pushing raw data (peak areas, retention times) to a dedicated project repository.
4. AI-Powered Data Analysis & Querying:
- The researcher accesses the platform and queries the AI agent using natural language: "Calculate the mean accuracy (% recovery) and intermediate precision (%RSD) for the 50 μg/mL validation samples."
- The AI agent, understanding the context, executes the following automated protocol:
- Data Retrieval: Identifies and retrieves the peak area data for all replicates at the 50 μg/mL level.
- Calculation of Accuracy: Calculates the mean measured concentration from a pre-established linear calibration curve. Accuracy is then calculated as:
(Mean Measured Concentration / 50 μg/mL) * 100[3] [5]. - Calculation of Precision: Calculates the standard deviation and %RSD of the measured concentrations for the five replicates. The %RSD is calculated as:
(Standard Deviation / Mean) * 100[5]. - Contextualization: The AI agent responds with: "For the 50 μg/mL samples (n=5), the mean accuracy is 98.5% recovery, and the intermediate precision is 1.8% RSD. These values are within our pre-defined acceptance criteria (Accuracy: 85-115%; Precision: <5% RSD)."
5. Validation and Reporting:
- The platform automatically generates a validation summary report, populating tables with the calculated results from all tested concentrations.
- The complete data pedigree—from raw instrument output to the final calculated values—is preserved and auditable within the platform, fulfilling regulatory requirements for data integrity [58] [3].
The convergence of centralized data platforms and Agentic AI marks a critical evolution in scientific informatics, directly addressing the pervasive challenge of data overload. For researchers and drug development professionals engaged in the meticulous work of method validation, precision, and accuracy verification, these technologies offer a path from being data managers to being data beneficiaries. By providing conversational access to contextualized, trustworthy data, these platforms enhance the reliability, traceability, and efficiency of research. They empower scientists to not only navigate but also master the complex data landscapes of modern laboratories, ensuring that the foundational principles of validation are upheld with greater rigor and insight than ever before.
Strategies for Robust Method Transfer and Outsourcing
Within the broader context of method validation, precision, and accuracy verification research, the successful transfer and outsourcing of analytical methods are critical pillars in the drug development lifecycle. For researchers, scientists, and drug development professionals, a failed technology transfer can lead to months of recovery effort, high expenditure, and a significant dent in investor trust [63]. Regulatory bodies emphasize that technology transfer activities form the basis for the manufacturing process, control strategy, and process validation [63]. This guide provides an objective comparison of core transfer methodologies and outsourcing frameworks, supported by structured data and protocols, to ensure robust and defensible results.
Core Method Transfer Approaches: A Comparative Analysis
A strategic, project-managed approach is non-negotiable for transferring product and process knowledge between development and manufacturing, whether internally or to an outsourcing partner [63]. The choice of transfer strategy is often determined by the specific project phase, regulatory requirements, and available resources.
Table 1: Comparative Analysis of Method Transfer Strategies
| Transfer Strategy | Core Methodology | Typical Application Context | Key Acceptance Criteria | Regulatory Considerations |
|---|---|---|---|---|
| Comparative Testing [64] | Identical sample batches are tested in parallel by both the sending and receiving units. | Most prevalent approach; suitable for most GMP testing transfers. | Agreement of results between laboratories as defined in a pre-established protocol. | Requires a detailed transfer protocol and report documenting procedural details and acceptance criteria. |
| Covalidation [64] | The receiving laboratory participates as part of the validation team, conducting experiments (e.g., for intermediate precision). | When GMP testing requires multiple laboratories; efficient for integrating a new site early. | Data generated demonstrates reproducibility and meets pre-defined validation parameters. | The receiving lab's activities are part of the overall validation study, requiring comprehensive documentation. |
| Revalidation [64] | The receiving laboratory performs a risk-based re-execution of parts of the original validation. | Optimal when the originating laboratory is unavailable for comparative testing. | Successful re-performance of selected validation parameters (e.g., accuracy, precision, specificity). | Justification for the extent of revalidation required must be documented based on a risk assessment. |
| Transfer Waiver [64] | A formal transfer is waived; the receiving lab performs a verification based on existing data and experience. | The procedure is standard (e.g., USP-NF) or the receiving lab has existing experience with the method. | Successful verification that the method works as expected in the receiving laboratory. | Requires robust justification based on the receiving unit's proven experience and records. |
Experimental Protocols for Method Transfer
The following protocols provide a framework for executing key transfer strategies, ensuring the process is meticulously planned, documented, and aligned with regulatory expectations.
Protocol for Comparative Testing
This protocol outlines the critical steps for the most common transfer approach [64].
- Protocol Development: A detailed technology transfer protocol is jointly developed and approved by both sending and receiving units. This document must list key personnel and responsibilities; materials, methods, and equipment; experimental design; and definitive acceptance criteria [63].
- Sample Selection and Shipment: Uniform, homogeneous, and stable batches of material (e.g., drug substance or product) are selected and shipped to the receiving laboratory under controlled conditions to maintain integrity.
- Parallel Testing: Both laboratories test the same samples using the transferred analytical method. The number of runs, replicates, and concentration levels (for bioanalytical assays) should be statistically justified.
- Data Analysis and Comparison: Data from both sites are collected and statistically compared against the pre-defined acceptance criteria. This often involves assessing the equivalence of results for critical quality attributes.
- Report Generation: A formal technology transfer report is issued, documenting the scope, methodology, and results, and providing a conclusion on the success of the transfer. This report serves as documented evidence for regulatory reviews [63].
Protocol for a Risk-Based Transfer (Revalidation)
When comparative testing isn't feasible, a risk-based revalidation is often the optimal path [64].
- Risk Assessment Initiation: A cross-functional team conducts a risk assessment of the analytical method. Failure Mode and Effects Analysis (FMEA) is a common tool to identify parameters critical to method performance.
- Scope Definition: Based on the risk assessment, the team defines which aspects of the original validation (e.g., precision, accuracy, robustness, specificity) need to be re-performed by the receiving laboratory.
- Partial Validation Execution: The receiving laboratory executes the agreed-upon validation experiments, following the same standard operating procedures as the originating lab.
- Data Review and Justification: Data from the partial validation is reviewed. Any deviations from the original validation data must be investigated and scientifically justified, demonstrating that the method remains suitable for its intended use in the new environment.
- Compilation of Comparability Report: The outcomes of the risk assessment and partial validation are compiled into a comparability report, which may also serve as the technology transfer report [63].
Visualization of Method Transfer Workflows
The following diagrams illustrate the logical flow of the overarching technology transfer process and the decision pathway for selecting the appropriate transfer strategy.
Technology Transfer Lifecycle
Transfer Strategy Selection
The Scientist's Toolkit: Essential Research Reagent Solutions
The integrity of any analytical method transfer hinges on the quality and consistency of critical reagents. Meticulous management of these materials is fundamental to achieving precision and accuracy.
Table 2: Key Reagents for Bioanalytical Method Transfer and Validation
| Reagent/Material | Critical Function | Considerations for Transfer |
|---|---|---|
| Reference Standards | Serves as the primary benchmark for identifying the analyte and constructing the calibration curve, directly impacting accuracy. | Must be of certified purity and quality. Sourcing, characterization data, and Certificate of Analysis (CoA) must be shared with the receiving unit. |
| Critical Reagents (e.g., antibodies, enzymes, ligands) | Essential for the specificity of the assay (e.g., immunoassays, cell-based assays). Binding affinity and specificity are paramount. | A robust plan for qualification, stability monitoring, and bridging studies is required if reagent batches are changed. |
| Calibration Curve Samples | Defines the analytical range and enables the quantitation of the analyte in unknown samples. | The preparation process and acceptance criteria for the curve (e.g., R², back-calculated accuracy) must be standardized. |
| Quality Control (QC) Samples | Act as internal proxies for study samples to monitor the assay's performance and accuracy during each run. | QC concentrations (low, mid, high) must be predefined. Their performance against acceptance criteria (e.g., ±15% bias) validates the run. |
| Matrix Samples (e.g., plasma, serum) | The biological material from which the analyte is extracted. Can cause matrix effects that interfere with detection. | The source and type of matrix (e.g., human, rat) must be consistent. Control (blank) matrix is required to demonstrate selectivity. |
Strategic Outsourcing Frameworks for Drug Development
Outsourcing, a strategic catalyst for growth, requires a disciplined framework to be effective, especially in a highly regulated environment [65] [66]. The approach varies significantly based on the company's demographics and needs.
Table 3: Outsourcing Strategies Aligned with Company Profile and Need
| Company Profile | Primary Outsourcing Driver | Recommended Strategic Posture | Critical Success Factors |
|---|---|---|---|
| Virtual Biotech [63] | Needs to outsource everything. | Comprehensive partnership with a CRO/CMO, treating them as an extension of the company. | Meticulous vendor selection, flawless communication, and robust quality/technical agreements. |
| Emerging Biotech [63] | Majority of key development stages and CGMP clinical manufacturing. | Strategic identification of core vs. non-core activities [65]; outsourcing to access expertise and reduce program risk. | Choosing a reliable partner who understands your goals and aligns with brand values [65]. |
| Established Biotech [63] | Access partner’s expertise, reduce risk, manage multiple product pipelines. | Hybrid model, mixing in-house and outsourced functions to optimize resource allocation and focus. | Performance monitoring, regular reviews, and adjusting the partnership to ensure continued value [65]. |
A critical first step for any company is selecting the right partner. This requires a clear and strategic approach, evaluating factors such as the provider's proven track record, technological capabilities, and quality systems [67]. Do not hide any process or analytical method issues from your Contract Manufacturing Organization (CMO); transparency is critical to avoiding delays and costs later on [63].
Furthermore, the outsourcing relationship must be governed by clear agreements. Service Level Agreements (SLAs) are the backbone of effective collaboration, going beyond basic terms to define clear standards, set measurable goals, and ensure mutual accountability [67]. These should be complemented by formal quality and technical agreements that are legally binding and define the technology transfer scope, deliverables, and responsibilities [63].
Strategic Selection: Choosing Between Validation, Verification, and Transfer
In pharmaceutical development, clinical diagnostics, and food safety testing, the reliability of analytical data is paramount. Method validation and method verification are two essential, distinct processes that ensure analytical methods are fit for their intended purpose, yet they are often confused [68]. Within a lifecycle approach to analytical procedures, validation is the comprehensive process of establishing that a method's performance characteristics are suitable for its intended application, typically for new methods [68]. In contrast, verification is the targeted process of confirming that a previously validated method performs as expected within a specific laboratory's environment, using its personnel, equipment, and reagents [69] [70].
Understanding the distinction is more than a technicality; it is a regulatory requirement that directly impacts data integrity, operational efficiency, and regulatory compliance. This guide provides an objective comparison to help researchers, scientists, and drug development professionals strategically implement these processes within their lab workflows.
Core Conceptual Differences
The fundamental difference lies in the questions each process answers. Method validation asks, "Are we developing the right method?" and "Is this method capable of producing reliable data for its intended purpose?" [71]. It is a process of proving and documenting that the method is capable of producing accurate, precise, and reliable results across its defined range [68]. Method verification, instead, asks, "Can we execute this already-validated method correctly in our lab?" Its purpose is to confirm that the validated performance can be achieved under actual conditions of use [68] [1].
The following workflow diagram illustrates the decision-making process for determining when each activity is required.
Direct Comparative Analysis: Scope, Application, and Regulation
The distinction between validation and verification manifests in their scope, timing, and regulatory demands. The following table provides a structured, point-by-point comparison essential for project planning.
Table 1: Comprehensive Comparison of Method Validation vs. Verification
| Aspect | Method Validation | Method Verification |
|---|---|---|
| Core Objective | Establish performance characteristics for a new method [68] | Confirm performance of an existing method in a new setting [68] [70] |
| Primary Question | "Are we building the method right?" [71] | "Can we run the method correctly?" [68] |
| Typical Scenarios | New in-house methods; significant modifications to compendial methods; methods for new products [68] | Adopting a USP/Ph. Eur. method; using a method from a Marketing Authorization dossier; method transfer between sites [68] |
| Regulatory Guidance | ICH Q2(R2); USP <1225> [68] | USP <1226>; ISO 16140-3 (for microbiology) [68] [72] |
| Timing in Workflow | During method development, prior to routine use [68] [70] | Before first use of a validated method within a specific laboratory [68] |
| Resource Intensity | High (time, cost, personnel) [70] | Moderate to Low [70] |
| Key Performance Characteristics Assessed | All relevant characteristics (e.g., Accuracy, Precision, Specificity, Linearity, Range, LOD, LOQ, Robustness) [4] | A subset of critical characteristics (e.g., Precision, Specificity, Accuracy for the specific sample matrix) [68] [69] |
Experimental Protocols and Performance Characteristics
The experimental protocols for validation are comprehensive and defined by guidelines like ICH Q2(R2). Verification involves a subset of these tests, chosen based on the method's nature and the laboratory's context [68] [69].
Protocols for Full Method Validation
For a quantitative impurity assay, the following validation protocol is typical. The corresponding workflow outlines the key experimental stages.
- Specificity/Selectivity: The ability to assess the analyte unequivocally in the presence of potential interferences (impurities, degradation products, matrix components) [4] [1]. Protocol: Inject individually: blank (excipients), placebo, analyte standard, and samples spiked with potential interferents. Resolution and peak purity are critical metrics.
- Linearity and Range: Linearity is the method's ability to produce results directly proportional to analyte concentration. The Range is the interval between upper and lower analyte levels with suitable precision, accuracy, and linearity [4] [1]. Protocol: Prepare a minimum of 5 concentrations, typically from 80% to 120% of the test concentration for assay. Analyze and plot response vs. concentration. Calculate regression line (e.g., by least squares); R² > 0.95 is often an acceptance criterion [4].
- Accuracy: The closeness of agreement between the measured value and a known reference value [4] [1]. Protocol for Drug Products: Spike a known amount of analyte (reference standard) into a synthetic mixture of the sample matrix (excipients). Perform the analysis and calculate recovery (%) of the known amount. Use at least 3 concentration levels with 3 replicates each [4].
- Precision: The degree of agreement among individual test results from repeated samplings. It has three tiers [4]:
- Repeatability: Precision under the same conditions over short time (e.g., 6 determinations at 100% concentration).
- Intermediate Precision: Variation within one lab (different days, analysts, equipment).
- Reproducibility: Precision between different labs (assessed in collaborative studies).
- Detection Limit (LOD) & Quantitation Limit (LOQ): LOD is the lowest detectable amount, while LOQ is the lowest quantifiable amount with acceptable precision and accuracy [4] [1]. Protocol (Signal-to-Noise): For chromatographic methods, a S/N ratio of 3:1 is generally acceptable for LOD, and 10:1 for LOQ [4].
- Robustness: A measure of the method's capacity to remain unaffected by small, deliberate variations in procedural parameters (e.g., mobile phase pH, temperature, flow rate) [1].
Protocols for Method Verification
For a compendial method (e.g., from USP), the laboratory must verify its suitability under actual conditions of use [69]. The extent of verification depends on the method's complexity, the sample, and the analyst's experience. Key activities include:
- Demonstrating Precision: Performing repeatability testing on the specific product to show the method delivers consistent results in the user's lab [68] [69].
- Confirming Specificity: Showing the method can accurately measure the analyte in the specific sample matrix, demonstrating freedom from interference [68] [69].
- Assessing Accuracy (as needed): For a finished dosage form, this may involve spiking the product with a known quantity of the analyte to confirm recovery is within acceptable limits [69].
Quantitative Data and Performance Metrics
The quantitative outcomes from validation and verification studies are judged against pre-defined acceptance criteria, which vary based on the method's type and application.
Table 2: Typical Acceptance Criteria for Key Performance Parameters
| Parameter | Typical Acceptance Criteria (e.g., for Assay of Drug Product) | Applicability in Verification |
|---|---|---|
| Accuracy (Recovery %) | Mean recovery of 98–102% [4] | Confirmed for the specific sample matrix |
| Precision (Repeatability) | RSD ≤ 1.0% for assay of drug product [4] | Confirmed (RSD meets compendial or predefined criteria) |
| Linearity (Correlation Coefficient R²) | R² > 0.95 [4] | Typically not re-evaluated |
| Range | Typically 80–120% of test concentration [4] | Confirmed that the sample concentration falls within the validated range |
| Specificity | Resolution of analyte peak from nearest potential interferent peak; Peak purity demonstrated. | Confirmed for the specific sample formulation |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of validation and verification studies depends on high-quality materials and reagents.
Table 3: Essential Materials for Method Validation and Verification
| Item | Function in Validation/Verification |
|---|---|
| Certified Reference Standards | Provides the known "true value" for establishing Accuracy and Linearity. Must be of known purity and identity [4]. |
| High-Purity Reagents & Solvents | Ensures baseline noise and interference are minimized, critical for assessing Specificity, LOD, and LOQ. |
| Well-Characterized Sample Matrix | For drug products, a placebo containing all excipients is essential for spiking studies to demonstrate Accuracy and Specificity in the relevant matrix [4]. |
| System Suitability Test (SST) Standards | A mixture of analytes and/or known impurities used to confirm the chromatographic system is performing adequately before and during the analysis, as required by regulatory expectations [68]. |
Choosing between method validation and verification is not a matter of preference but a strategic decision dictated by the method's origin and status. Validation is the foundational process for novel methods, requiring significant resources to establish fitness-for-purpose. Verification is the efficiency-focused process for adopting established methods, requiring laboratories to demonstrate operational competence [68] [70].
A hybrid approach is often employed across an organization: R&D laboratories frequently engage in full method validation, while Quality Control (QC) laboratories routinely perform method verification when implementing compendial or transferred methods. By understanding these distinctions and implementing the respective protocols rigorously, laboratories can ensure data integrity, maintain regulatory compliance, and optimize their analytical workflows for efficiency and reliability.
When is Full Validation Required? Scenarios for Novel Methods and Submissions
In laboratory and clinical research, ensuring the reliability of analytical methods is fundamental to data integrity and regulatory compliance. Two cornerstone processes in this endeavor are method validation and method verification. Though sometimes used interchangeably, they serve distinct purposes and are required under different circumstances [70].
Method validation is a comprehensive, documented process that proves an analytical method is acceptable for its intended use. It establishes the performance characteristics and limitations of a method and its domain of operational parameters [70] [73]. Method verification, in contrast, is a streamlined assessment to confirm that a previously validated method performs as expected under a specific laboratory's conditions, such as when adopting a manufacturer-approved or compendial method like those from the USP or AOAC [70] [73] [74].
The choice between full validation and verification is not arbitrary; it is dictated by the method's origin, novelty, and its role in regulatory submissions. This guide objectively compares these processes and outlines the specific scenarios where full validation is mandatory.
Key Comparisons: Validation vs. Verification
Understanding the fundamental differences between validation and verification is crucial for selecting the correct pathway. The table below provides a structured comparison of their core attributes.
Table 1: Core Differences Between Method Validation and Method Verification
| Comparison Factor | Method Validation | Method Verification |
|---|---|---|
| Purpose & Scope | Comprehensive evaluation to establish performance characteristics for a new or significantly modified method [70] [73]. | Limited assessment to confirm a validated method performs as claimed in a user's specific laboratory [70] [73]. |
| When Required | Development of new methods; significant modifications; Laboratory-Developed Tests (LDTs); novel assays [70] [73]. | Adoption of standard, compendial (e.g., USP, EPA), or manufacturer-approved methods [70] [74]. |
| Regulatory Driver | Required for new drug applications, clinical trials, and novel assay development [70]. | Acceptable for implementing standard methods in established workflows; required by ISO/IEC 17025 for such methods [70]. |
| Typical Duration | Weeks or months, depending on method complexity [70]. | Can be completed in days, enabling rapid deployment [70]. |
| Parameters Assessed | Full suite: Accuracy, Precision, Specificity, Linearity, Range, Robustness, LOD, LOQ [73] [3] [74]. | Limited set, typically focusing on Accuracy and Precision to confirm manufacturer claims [73] [11]. |
Mandatory Scenarios for Full Method Validation
Full validation is non-negotiable in several critical scenarios within the drug development and diagnostic pipeline. The following workflow diagram outlines the decision-making process for determining when full validation is required.
Development of Novel Analytical Methods
Any newly developed analytical method, such as a novel HPLC assay for a new chemical entity or a new immunoassay for a novel biomarker, requires full validation before it can be used to generate reportable data [70] [73]. This process generates the foundational evidence that the method is fit for its intended purpose.
Laboratory-Developed Tests (LDTs) and Significant Modifications
Laboratory-Developed Tests, which are in-house validated diagnostic assays, necessitate full validation [73]. Similarly, any significant modification to an existing validated method—such as changes to the sample preparation, critical instrumentation, or analytical principle—triggers a re-validation requirement to ensure the changes have not adversely affected method performance [74].
Methods for Regulatory Submissions
In highly regulated industries like pharmaceuticals, full method validation is essential for any method used to support regulatory submissions for new drug applications (e.g., to the FDA or EMA), clinical trials, or diagnostic test approvals [70] [75]. Regulatory bodies require documented evidence that the method is scientifically sound and reliable.
Application to New Matrices or Analytes
Applying an existing method to a new sample matrix (e.g., moving from plasma to urine) or for a new analyte requires full validation to demonstrate the method's performance in the new context [76]. The new matrix may introduce interferences or affect extraction efficiency, which must be thoroughly evaluated.
Experimental Protocols for Full Validation
Full validation requires a systematic experimental approach to evaluate key performance parameters against pre-defined acceptance criteria. The following protocols are based on established guidelines from organizations like the Clinical and Laboratory Standards Institute (CLSI) and the International Council for Harmonisation (ICH) [73] [11] [74].
Accuracy Assessment
Objective: To establish the closeness of agreement between the measured value and a known reference or true value [73] [3].
Protocol:
- Method Comparison: Perform method comparison studies using at least 40 patient samples across the reportable range, comparing results to a reference method [73].
- Spike Recovery: For chromatographic assays, spike the analyte of interest into a blank matrix at three concentrations (e.g., 80%, 100%, 120% of the target) and analyze in triplicate. Calculate percent recovery [3].
- Data Analysis: Use regression analysis (e.g., Passing-Bablok) to calculate bias and ensure it falls within the allowable total error (TEa) [73].
Precision Evaluation
Objective: To measure the random error and assess the consistency of results under specified conditions [73] [11].
Protocol (CLSI EP05-A2 for full validation):
- Experimental Design: Test at least two concentrations (normal and pathological). Run each level in duplicate, with two runs per day, separated by at least two hours, over 20 days [11].
- Data Analysis: Use analysis of variance (ANOVA) to calculate standard deviation (SD) and coefficient of variation (CV) for:
- Repeatability (Within-run): Variation under identical conditions.
- Within-laboratory Precision (Total): Combined within-run and between-run (day-to-day) variation [11].
- Acceptance: The calculated imprecision should be less than the allowable imprecision based on the intended clinical or analytical use.
Table 2: Key Performance Parameters and Their Validation Experiments
| Performance Parameter | Experimental Goal | Typical Validation Experiment | Common Acceptance Criteria |
|---|---|---|---|
| Accuracy | Measure systematic error (bias) [3] | Method comparison with 40+ patient samples or spike/recovery [73] [3] | Bias < allowable total error (TEa) [73] |
| Precision | Measure random error (impression) [11] | 20-day replication study per CLSI EP05-A2 [11] | CV% < claimed or required CV% [11] |
| Linearity & Reportable Range | Verify results are proportional to analyte concentration [73] | Analyze at least 5 concentrations spanning the claimed range [73] | Linear regression R² > 0.99; total error within TEa at each level [73] |
| Analytical Sensitivity (LoD/LoQ) | Determine the lowest detectable/quantifiable amount [73] | Analyze 20+ replicates of blank and low-level samples; LoB + 1.65SD [73] | CV% at LoQ < allowable limit (e.g., 20%) [73] |
| Specificity | Ensure the method measures only the intended analyte [74] | Analyze samples with and without potential interferents (e.g., hemolysis) [73] | No significant bias from interferents [73] |
Establishing Analytical Sensitivity (LoD and LoQ)
Objective: To determine the lowest concentration of an analyte that can be reliably detected (Limit of Detection, LoD) and quantified (Limit of Quantification, LoQ) [73].
Protocol:
- Limit of Blank (LoB): Test at least 20 replicate blank samples. LoB = mean blank + 1.65 * SDblank.
- Limit of Detection (LoD): Test at least 20 replicate samples with low analyte concentration. LoD = LoB + 1.65 * SDlow concentration sample.
- Limit of Quantification (LoQ): Test at least 30 replicates at a low concentration. The LoQ is the lowest level where both bias and imprecision (CV%) meet predefined acceptability criteria for quantitative measurement [73].
The Scientist's Toolkit: Essential Reagents and Materials
Successful method validation relies on high-quality, traceable materials. The following table details essential items for validation experiments.
Table 3: Essential Research Reagent Solutions for Validation Studies
| Reagent / Material | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Certified Reference Standard | Serves as the primary calibrator with known purity; used to prepare samples for accuracy, linearity, and precision studies [3]. | Documented purity and stability; certificate of analysis from a certified supplier (e.g., NIST, USP) [3]. |
| Quality Control (QC) Materials | Used to monitor assay performance during precision and robustness studies; should be different from calibrators [11]. | Commutability with patient samples; well-characterized target value and acceptable range; stable for the duration of the study [11]. |
| Appropriate Biological Matrix | The material in which the analyte is measured (e.g., plasma, serum, urine). Used to prepare calibration standards and QC samples [3]. | Should match the intended patient sample matrix as closely as possible; checked for absence of endogenous analyte or interferents for recovery experiments [3]. |
| Interferent Stocks | Used in specificity experiments to challenge the method and ensure it is free from interference [73]. | High-purity substances (e.g., bilirubin, hemoglobin, lipids) to simulate common biological interferents; prepared at clinically relevant concentrations [73]. |
The decision to perform a full method validation is governed by clear regulatory and scientific principles. It is mandatory for novel methods, Laboratory-Developed Tests, significant modifications, and methods supporting critical regulatory submissions. In these contexts, verification is insufficient. A rigorous validation protocol, assessing accuracy, precision, linearity, sensitivity, and specificity against pre-defined criteria, generates the objective evidence required to prove a method is fit-for-purpose. This foundational process ensures the integrity, reliability, and regulatory acceptance of the data produced, which is paramount in pharmaceutical development and clinical diagnostics.
The Role of Verification for Compendial and Standardized Methods
In the tightly regulated environments of pharmaceutical development and quality control, demonstrating the reliability of analytical methods is paramount. Within the broader thesis on method validation, precision, and accuracy research, method verification stands as a critical, distinct process. It is the practice that ensures established testing procedures perform as intended within a specific laboratory's unique operating environment [77]. For researchers and scientists, understanding verification is essential for efficiently deploying compendial methods—those published in authoritative sources like the United States Pharmacopeia (USP), European Pharmacopoeia (Ph.Eur.), or Japanese Pharmacopoeia (JP)—without the need for extensive re-development [1] [77].
The core objective of method verification is to provide documented evidence that a previously validated method is suitable for its intended use under actual conditions of use [1] [68]. This involves confirming that the method's performance characteristics, which were proven during the initial validation, can be achieved by the user's laboratory with its specific analysts, equipment, and reagents [70]. This process is not a repetition of the full validation but a targeted confirmation of reliability in a new context [78] [68].
Verification vs. Validation: A Critical Distinction
A clear understanding of the difference between method validation and method verification is fundamental for drug development professionals. The choice between them is dictated by the origin and history of the analytical method. The following workflow outlines the decision-making process for implementing a new analytical procedure.
Comparative Analysis: Scope and Application
The table below summarizes the key distinctions between these two processes, which are often confused but serve different purposes in the method lifecycle.
Table 1: Key Differences Between Method Validation and Verification
| Comparison Factor | Method Validation | Method Verification |
|---|---|---|
| Objective | Establish performance characteristics for a new method [1] [79] | Confirm suitability of a pre-validated method in a user's lab [77] [68] |
| When Performed | Method development; significant modification [70] [68] | Adoption of a compendial or transferred method [70] [78] |
| Scope | Comprehensive assessment of all relevant performance parameters [1] [79] | Limited assessment of critical parameters to confirm performance [77] [80] |
| Regulatory Basis | ICH Q2(R2), USP <1225> [79] [68] | USP <1226>, Ph.Eur. General Notices [77] [68] |
| Typical Parameters | Accuracy, Precision, Specificity, LOD/LOQ, Linearity, Range, Robustness [1] [79] | Accuracy, Precision, Specificity (as applicable) and System Suitability [77] [80] |
Experimental Protocols for Verification
The verification process is a structured sequence of activities designed to efficiently demonstrate method suitability. The following workflow provides a high-level overview of the key stages, from initial planning to final approval.
Core Performance Parameters and Testing Methods
The verification exercise focuses on a subset of validation parameters, selected based on the method's complexity and intended use [77] [78]. The experiments are designed to be sufficient to confirm that the method works for the specific product in the actual laboratory.
Table 2: Key Verification Parameters and Experimental Protocols
| Parameter | Experimental Protocol | Acceptance Criteria |
|---|---|---|
| Accuracy | Analyze a sample of known concentration (e.g., reference standard) and calculate the percentage recovery [79] [78]. Alternatively, spike the product with a known amount of analyte [79]. | Recovery should be within established limits, typically close to 100% [1]. |
| Precision | Perform at least five replicate measurements of a homogeneous sample [78]. Calculate the standard deviation (SD) and relative standard deviation (RSD) [79]. | The RSD (coefficient of variation) meets the pre-defined level suitable for the method [1] [79]. |
| Specificity | Demonstrate that the method can unequivocally quantify the analyte in the presence of potential interferences like impurities, excipients, or matrix components [1] [79]. | The analyte response is unaffected by the presence of expected sample components. |
| Linearity & Range | Prepare and analyze analyte at a minimum of five concentration levels across the claimed range [78]. Plot response versus concentration and calculate the correlation coefficient [79]. | The correlation coefficient (r) is typically ≥ 0.995 [1]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful verification relies on high-quality, traceable materials. The following table details key solutions and materials required for the featured experiments.
Table 3: Essential Research Reagent Solutions for Method Verification
| Reagent / Material | Function in Verification |
|---|---|
| Certified Reference Standard | Serves as the primary benchmark for establishing accuracy and preparing calibration standards for linearity and precision studies [79]. |
| System Suitability Test Mixtures | Used to verify that the total analytical system (instrument, reagents, columns) is performing adequately before proceeding with sample analysis [68]. |
| Control Samples | Characterized samples (e.g., placebo, blank, spiked sample) used to monitor precision and accuracy during the verification process [77] [78]. |
| High-Purity Reagents & Solvents | Ensure that impurities do not interfere with the assessment of specificity, baseline noise, detection limit, or accuracy [79]. |
Regulatory Framework and Compendial Context
Method verification is a formal requirement under various regulatory standards and pharmacopoeias. The United States Pharmacopeia (USP) states that users of compendial methods "are not required to validate the accuracy and reliability of these methods, but merely verify their suitability under actual conditions of use" [77] [79]. This principle is echoed by other major pharmacopoeias, including the European (Ph.Eur.) and Japanese (JP) Pharmacopoeias, which all consider their methods to be pre-validated [77].
The level of verification required can depend on the complexity of the method. For instance, technique-dependent methodologies such as loss on drying, pH, or residue on ignition may not require extensive verification beyond analyst training [77]. In contrast, chromatographic methods (e.g., HPLC) should, at a minimum, meet system suitability requirements and may require checks of accuracy and precision [77]. For protein products, verification of physical tests (e.g., subvisible particles, osmolality) presents specific challenges, where precision may be assessed through repeated testing or by comparing analyst results [80].
Within the rigorous framework of pharmaceutical analysis, method verification is not a shortcut but a strategically vital process. It efficiently leverages the extensive validation work conducted by compendial bodies and manufacturers, translating it into demonstrable reliability within a local laboratory context. For researchers and drug development professionals, mastering verification protocols ensures regulatory compliance, optimizes resource allocation, and, most importantly, provides confidence that compendial and standardized methods will consistently yield accurate and precise results for their specific products. This confirmation is the final, critical link in the chain of evidence that underpins product quality and patient safety.
Establishing Acceptance Criteria for Transfer and Verification Protocols
This guide provides an objective comparison of method transfer and verification protocols, framing them within the broader context of method validation to ensure precision and accuracy in scientific research. It is designed to support researchers, scientists, and drug development professionals in establishing robust acceptance criteria.
In regulated product testing, demonstrating the reliability of analytical methods is paramount for regulatory acceptance. The terms validation, verification, and transfer represent distinct but interconnected processes within a method's lifecycle [1].
Method Validation is the foundational process of establishing, through laboratory studies, that the performance characteristics of a method meet the requirements for its intended analytical applications [1]. It is typically performed on new methods and evaluates characteristics such as Accuracy, Precision, Specificity, and Linearity [1].
Method Verification is the process used when a laboratory needs to demonstrate that it can successfully perform a compendial or previously validated method. For United States Pharmacopeia (USP) methods, while full re-validation is not required, the suitability of the method must be verified under the laboratory's actual conditions of use [1].
Method Transfer is the qualified process of moving a validated method from one laboratory to another (e.g., from R&D to a quality control lab). The receiving laboratory demonstrates that the method can be performed with acceptable precision and accuracy by its personnel [1].
Experimental Protocols for Comparative Analysis
A rigorous, data-driven approach is essential for comparing the performance of transfer and verification protocols. The following methodology outlines a standard framework for such evaluations.
Experimental Workflow for Protocol Assessment
The diagram below illustrates the logical workflow for conducting a comparative assessment of transfer and verification protocols.
Core Performance Metrics and Assessment
The evaluation of both transfer and verification protocols hinges on measuring key analytical performance characteristics. The following table summarizes the core metrics and their definitions, which are critical for establishing acceptance criteria [1].
Table 1: Core Analytical Performance Characteristics for Protocol Assessment
| Performance Characteristic | Definition | Role in Protocol Assessment |
|---|---|---|
| Accuracy | The closeness of test results to the true value. | Ensures the method produces correct results in the receiving lab. |
| Precision | The degree of agreement among individual test results from repeated samplings. | Confirms the method's reproducibility by new analysts. |
| Specificity | The ability to measure the analyte clearly in the presence of potential interferences. | Verifies the method's selectivity is maintained. |
| Linearity | The ability to produce results directly proportional to analyte concentration. | Demonstrates the method's response over the required range. |
| Range | The interval between upper and lower analyte levels for suitable precision and accuracy. | Confirms the validated range is achievable. |
| Robustness | The capacity to remain unaffected by small, deliberate procedural variations. | Assesses the method's resilience to minor operational changes. |
Detailed Experimental Methodology
To generate the comparative data, a standardized experimental protocol should be followed.
- Sample Preparation: A homogenous sample of a drug product is prepared. For biomarker assays, this involves using actual biological samples containing the endogenous biomarker at varying levels, as spiked reference standards are not applicable [81].
- Instrumental Analysis: The same set of prepared samples is analyzed by both the transferring (sending) laboratory and the receiving laboratory. This is typically performed using High-Performance Liquid Chromatography (HPLC) systems.
- Data Collection: Each laboratory conducts multiple independent assays (e.g., n=6) across different days to capture both intra- and inter-day precision.
- Statistical Analysis: Results from both laboratories are compiled. Key statistical parameters are calculated, including mean accuracy (as % of reference value), standard deviation (SD), relative standard deviation (RSD or %CV) for precision, and linear regression analysis (R²) for the calibration curve.
Comparative Performance Data and Results
The following section presents synthesized quantitative data from a model study comparing a successful method transfer against a verification exercise for a hypothetical Active Pharmaceutical Ingredient (API).
Quantitative Performance Comparison
The table below provides a side-by-side comparison of key performance metrics for the transfer and verification protocols, based on the experimental methodology described.
Table 2: Comparative Performance Data for Transfer vs. Verification Protocols
| Analytical Parameter | Transfer Protocol (Sending Lab) | Transfer Protocol (Receiving Lab) | Verification Protocol (Receiving Lab) | Pre-defined Acceptance Criteria |
|---|---|---|---|---|
| Accuracy (% Recovery) | 99.8% | 100.2% | 99.5% | 98.0% - 102.0% |
| Precision (%RSD) | 0.9% | 1.1% | 1.3% | ≤ 2.0% |
| Linearity (R²) | 0.9995 | 0.9991 | 0.9989 | ≥ 0.998 |
| Specificity | No interference detected | No interference detected | No interference detected | No interference |
| Assay Range (mg/mL) | 10 - 150% | 10 - 150% | 20 - 130% | 10 - 150% |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of transfer and verification studies relies on specific, high-quality materials. The following table details key reagents and their functions in the context of these protocols.
Table 3: Essential Research Reagents and Materials for Protocol Studies
| Reagent / Material | Function / Explanation | Criticality for Success |
|---|---|---|
| Certified Reference Standard | A highly characterized material with a certified purity; used as the primary benchmark for calculating Accuracy. | High: The cornerstone for all quantitative measurements. |
| System Suitability Test Mixture | A mixture of analytes and potential impurities; used to verify chromatographic system performance before analysis. | High: Ensures the instrumental setup is valid for its intended use. |
| Placebo/Blank Matrix | The formulation or biological matrix without the active analyte; critical for demonstrating Specificity and absence of interference. | High: Directly supports the key parameter of Specificity. |
| Stressed/Degraded Samples | Samples subjected to forced degradation (e.g., heat, light, acid); used to prove the method can resolve the analyte from its degradation products. | Medium-High: Provides evidence for method selectivity and stability-indicating properties. |
| Quality Control (QC) Samples | Samples with known concentrations (low, mid, high) prepared independently from the calibration standards; used to monitor the assay's performance during the run. | High: Acts as an in-study check of accuracy and precision. |
Establishing clear, pre-defined acceptance criteria is the critical link between the theoretical framework of method validation and the practical application of methods in drug development. As demonstrated through the comparative data, both transfer and verification protocols serve to provide documentary evidence that a method functions as intended in a new operational environment. For method transfer, this involves a direct comparison of data between two laboratories, while verification focuses on the receiving laboratory's ability to meet the method's original validated characteristics. A rigorous, metrics-driven approach, centered on core parameters like accuracy, precision, and specificity, ensures the integrity of analytical data, supports regulatory compliance, and ultimately safeguards product quality.
Conclusion
The strategic application of method validation and verification is paramount for ensuring data integrity, regulatory compliance, and patient safety in pharmaceutical development. The key takeaways underscore the necessity of a science- and risk-based lifecycle approach, the growing influence of digital transformation through AI and automation, and the critical distinction between validating a new method and verifying an established one. Looking ahead, the integration of Real-Time Release Testing (RTRT), continuous process verification, and digital twin technology will further reshape the analytical landscape. For biomedical and clinical research, these evolving practices promise to accelerate the development of complex therapies, enhance manufacturing agility, and build a more robust foundation for the medicines of the future.
References
- 1. Method Validation Vs. Verification - A Simple Breakdown [https://cptclabs.com/method-validation-vs-verification/]
- 2. A Review: Comparison of ICH Guidelines on Analytical Method... [https://www.linkedin.com/pulse/review-comparison-ich-guidelines-analytical-method-usp-shaikh-wzfjc]
- 3. Accuracy, Precision, and Reliability of Chemical Measurements in Natural Products Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3026088/]
- 4. Performance Characteristics In Analytical Method Validation [https://gmpinsiders.com/performance-characteristics-method-validation/]
- 5. Validation of Analytical Methods | IntechOpen [https://www.intechopen.com/chapters/57909]
- 6. ( ICH ) Validation of Analytical Procedures: An... | QbD Group Q 2 R 2 [https://www.qbdgroup.com/en/blog/ich-q2r2-validation-of-analytical-procedures-an-overview-of-the-revised-guideline/]
- 7. FDA publishes Q2(R2) and Q14 Guidelines - ECA Academy [https://www.gmp-compliance.org/gmp-news/fda-publishes-q2r2-and-q14-guidelines]
- 8. Analytical procedure development - Scientific ICH Q 14 guideline [https://www.ema.europa.eu/en/ich-q14-analytical-procedure-development-scientific-guideline]
- 9. News about GMP/cGMP - GMP-Verlag: EMA: Comments on Draft ICH Q2(R2) and ICH Q14 Published [https://www.gmp-publishing.com/content/en/gmp-news/news-about-gmp-cgmp/d/ema-comments-on-draft-ich-q2-r2-and-ich-q14-published]
- 10. EMA vs FDA Expectations on Process Validation | Pharmaguideline [https://www.pharmaguideline.com/2025/07/ema-vs-fda-expectations-on-process-validation.html]
- 11. Evaluating Assay Precision - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556577/]
- 12. ALCOA …with an A for Accuracy [https://www.a3p.org/en/alcoa-accuracy/]
- 13. + ALCOA : A Principles to GxP Data Integrity | IntuitionLabs Guide [https://intuitionlabs.ai/articles/alcoa-plus-gxp-data-integrity]
- 14. in Life Sciences and Pharmaceutical... - TotalLab ALCOA Principles [https://totallab.com/resources/alcoa-principles/]
- 15. Guidelines for Research Data Integrity (GRDI) | Scientific Data [https://www.nature.com/articles/s41597-024-04312-x]
- 16. ALCOA, ALCOA+ and ALCOA++ Principles | Ensuring Data Integrity in Pharmaceuticals | Pharmaguideline [https://www.pharmaguideline.com/2018/12/alcoa-to-alcoa-plus-for-data-integrity.html]
- 17. Alcoa Validation Data | NNIT [https://slcontrols.com/en/what-is-alcoa-and-why-is-it-important-to-validation-and-data-integrity/]
- 18. Data Accuracy in 2025: What It Is & How to Ensure | Airbyte [https://airbyte.com/data-engineering-resources/data-accuracy]
- 19. Leading Pharmaceutical Validation Trends for 2025 [https://www.ellab.com/blog/transforming-the-industry-landscape-leading-pharmaceutical-validation-trends-for-2025/]
- 20. Essential Data Integrity Best Practices for 2025 [https://atlan.com/data-integrity-best-practices/]
- 21. Understanding ICH Quality Q Management | Scilife 9 Risk [https://www.scilife.io/blog/ich-q9-quality-risk-management]
- 22. - Risk USFDA Inspections Based ... - Laafon Galaxy Pharmaceuticals ICH [https://laafon.com/risk-based-usfda-inspections-ich-q9/]
- 23. Establishing Acceptance Criteria for Analytical Methods | BioPharm International [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 24. Paradigm Shift in Drug Development: Analytical Quality by Design and Analytical Procedure Life Cycle | Quality Matters | U.S. Pharmacopeia Blog [https://qualitymatters.usp.org/paradigm-shift-drug-development-analytical-quality-design-and-analytical-procedure-life-cycle]
- 25. Implementation of the QbD Approach to the Analytical Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12059909/]
- 26. Quality by Design for Analytical Methods: Implications for Method Validation and Transfer [https://www.pharmtech.com/view/quality-design-analytical-methods-implications-method-validation-and-transfer]
- 27. Quality by design in analytical method developmentpptx | PPTX [https://www.slideshare.net/slideshow/quality-by-design-in-analytical-method-developmentpptx/251481296]
- 28. QbD approach to HPLC method development and validation of ceftriaxone sodium | Future Journal of Pharmaceutical Sciences | Full Text [https://fjps.springeropen.com/articles/10.1186/s43094-021-00286-4]
- 29. Implementation of QbD Approach to the Analytical Method Development and Validation for the Estimation of Metformin Hydrochloride in Tablet Dosage Forms by HPLC - PubMed [https://pubmed.ncbi.nlm.nih.gov/35745760/]
- 30. QbD Based Analytical Method Development and Validation for the Estimation of Remogliflozin etabonate and Vildagliptin in Bulk and in Their Dosage Form | Journal of Chemical Health Risks [https://www.jchr.org/index.php/JCHR/article/view/5213]
- 31. -based QbD and AGREE-guided validation of... development [https://link.springer.com/article/10.1007/s44371-025-00319-4]
- 32. Design of Experiments in Pharmaceutical Development | Pharmaceutical Chemistry Journal [https://link.springer.com/article/10.1007/s11094-019-02070-4]
- 33. 5.1.2. What are the uses of DOE? [https://www.itl.nist.gov/div898/handbook/pri/section1/pri12.htm]
- 34. Design of experiments (DoE) in pharmaceutical development - PubMed [https://pubmed.ncbi.nlm.nih.gov/28166428/]
- 35. Design of Experiments (DoE), a valuable tool in (bio)pharmaceutical product, process and test method development [https://www.vennlifesciences.com/articles-and-research/design-of-experiments-doe-blog/]
- 36. Comparative DOE Optimization Criteria [https://www.numberanalytics.com/blog/comparative-doe-optimization-criteria]
- 37. Pharmaceutical Method ... - Laafon Galaxy Pharmaceuticals Validation [https://laafon.com/what-is-method-validation/]
- 38. Trends In Pharmaceutical Analytical 2025 Development... Methods [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 39. Design of Experiments (DoE) | SPT Labtech [https://www.sptlabtech.com/applications/design-of-experiments-doe]
- 40. Solved: method : % bias and recovery values from validation ? DoE [https://community.jmp.com/t5/Discussions/method-validation-bias-and-recovery-values-from-DoE/td-p/846568]
- 41. Ultrahigh-pressure liquid chromatography-mass spectrometry: An overview of the last decade - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0165993619301700]
- 42. Optimizing Ultra - High - Performance ... Liquid Chromatography [https://www.intechopen.com/chapters/1188571]
- 43. LC-MS (Ultra Performance Liquid Chromatography- High Resolution Mass Spectrometry) - Microtrace [https://www.microtrace.com/technique/uplc-hrms/]
- 44. Applications of Ultra High-Performance Liquid Chromatography Coupled with High-Resolution Mass Spectrometry | IntechOpen [https://www.intechopen.com/chapters/1191452]
- 45. Ultra high performance liquid chromatography-time-of-flight high... [https://pubmed.ncbi.nlm.nih.gov/25262032/]
- 46. Advancing Food Analysis with Ultrahigh-Pressure Liquid Chromatography and High-Resolution Mass Spectrometry | LCGC International [https://www.chromatographyonline.com/view/advancing-food-analysis-ultrahigh-pressure-liquid-chromatography-and-high-resolution-mass-spectrom-0]
- 47. Determination of Seventeen Phytocannabinoids in Various Matrices by... [https://www.chromatographyonline.com/view/determination-seventeen-phytocannabinoids-various-matrices-uhplc-hrmsms]
- 48. Validation, Monitoring, and Verification: A Comprehensive Comparison – Enhancing Your Business Performance [https://leanmanufacturing.online/validation-monitoring-and-verification-a-comprehensive-comparison/]
- 49. Validation, Monitoring And Verification Processes Critical To Effectiveness Of Food Safety Inspection Systems | Manufacturing.net [https://www.manufacturing.net/safety/article/13166776/validation-monitoring-and-verification-processes-critical-to-effectiveness-of-food-safety-inspection-systems]
- 50. Validation, Verification, Monitoring: Testing Inspection Devices - Sesotec [https://www.sesotec.com/na/en-US/resources/blog/how-to-test-foreign-material-detection-systems-validation-verification-monitoring]
- 51. The Hidden Risks in Analytical Method Validation [https://pharmuni.com/2025/05/16/the-hidden-risks-in-analytical-method-validation/]
- 52. Key Risks and Solutions in Method Validation [https://www.linkedin.com/pulse/key-risks-solutions-method-validation-pharcell-umsnf]
- 53. Laboratory Validation ... - Zamann Pharma Support GmbH Method [https://zamann-pharma.com/2025/04/29/laboratory-validation-method-from-basics-to-best-practices/]
- 54. A practical guide to validation and verification of analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S006524231930006X]
- 55. Navigating the Complexities of the Cell Landscape... and Gene Therapy [https://www.pharmacytimes.com/view/navigating-the-complexities-of-the-cell-and-gene-therapy-landscape-insights-from-the-2025-advanced-therapies-report]
- 56. Report Looks at Industry Challenges... 2025 Cell and Gene Therapy [https://www.targetedonc.com/view/2025-cell-and-gene-therapy-report-looks-at-industry-challenges-how-to-expand-nationally]
- 57. Forecast For Advanced 2025 Therapies [https://www.cellandgene.com/doc/2025-forecast-for-advanced-therapies-0001]
- 58. SaaS 2.0 & Agentic AI : Powering the Future of... | Technology Networks [https://www.technologynetworks.com/informatics/white-papers/ai-powered-lab-platforms-from-data-overload-to-data-fluency-401093]
- 59. Top 10: Data Platforms | Technology Magazine [https://technologymagazine.com/top10/top-10-data-platforms]
- 60. AI Data Platform for Enterprise Agentic AI | NVIDIA [https://www.nvidia.com/en-us/data-center/ai-data-platform/]
- 61. Choosing the Ideal Storage Solution for AI Applications [https://www.walturn.com/insights/choosing-the-ideal-storage-solution-for-ai-applications]
- 62. Top 12 AI Platforms for Business in 2025 [https://www.getguru.com/reference/ai-platforms]
- 63. Modern Technology Transfer Strategies for Biopharmaceutical... [https://www.bioprocessintl.com/risk-management/modern-technology-transfer-strategies-for-biopharmaceutical-companies]
- 64. CRO | Bioanalysis laboratory | Method & Development Transfer [https://www.biotrial.com/solutions-services/bioanalysis/method-development-method-transfer/]
- 65. Best Breakthrough Outsourcing In Strategies For Growth 2025 [https://syspree.com/blog/outsourcing-strategies-in-2025/]
- 66. What Is Outsourcing ? Definition, Types, and Strategies for 2025 [https://www.shopify.com/id/blog/what-is-outsourcing]
- 67. To Transform Your Operations in Outsourcing Strategies 2025 [https://www.linkedin.com/pulse/outsourcing-strategies-transform-your-operations-2025-i4skc]
- 68. Difference Between Validation And Verification Of Analytical Methods [https://gmpinsiders.com/method-validation-vs-verification/]
- 69. Method Verification Versus Method Validation [https://www.linkedin.com/pulse/method-verification-versus-validation-pharcell-9xlzf]
- 70. : Which is... | Lab Manager Method Validation vs Method Verification [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 71. What is Verification (V&V) Meaning in vs Validation 2025 [https://thetechsmarket.com/verification-vs-validation/]
- 72. Method validation and method verification [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 73. Comprehensive Guide to Validation and Verification Based on CLSI Guidelines – Diagnostics Edge [https://tdxedge.com/2025/01/25/comprehensive-guide-to-validation-and-verification-based-on-clsi-guidelines/]
- 74. Frequently Asked Questions about Method | Ofni Systems Validation [https://www.ofnisystems.com/services/method-validation/frequently-asked-questions-about-method-validation/]
- 75. FDA Validation Rules for Submission Data: Avoid Costly Mistakes! - ProRelix Research [https://prorelixresearch.com/fda-validation-rules-for-submission-data/]
- 76. in digital forensics (accessible) - GOV.UK Method validation [https://www.gov.uk/government/publications/method-validation-in-digital-forensics/method-validation-in-digital-forensics-accessible]
- 77. Verifying Compendial Methods | Pharmaceutical Technology [https://www.pharmtech.com/view/verifying-compendial-methods]
- 78. ISO 15189:2022 Method ‑Validation & Verification ... - Qse academy [https://www.qse-academy.com/iso-151892022-method%E2%80%91validation-verification-templates/]
- 79. General Chapters: <1225> VALIDATION OF COMPENDIAL METHODS [http://pharmacopeia.cn/v29240/usp29nf24s0_c1225.html]
- 80. : Suitability Compendial , Challenges and... Methods Verification [https://pubmed.ncbi.nlm.nih.gov/32295862/]
- 81. Understanding Biomarker Method : Validation & Accuracy ... Precision [https://www.linkedin.com/pulse/understanding-biomarker-method-validation-xyhhe]