Coordination Environment Analysis in Drug Development: Techniques, Applications, and Regulatory Frontiers
This article provides a comprehensive overview of coordination environment analysis techniques for researchers, scientists, and drug development professionals.
Coordination Environment Analysis in Drug Development: Techniques, Applications, and Regulatory Frontiers
Abstract
This article provides a comprehensive overview of coordination environment analysis techniques for researchers, scientists, and drug development professionals. It explores the foundational principles of systems-level coordination, from molecular drug-target interactions to the regulatory frameworks governing AI and complex data. The content details advanced methodological applications, including electroanalysis and network modeling, for practical use in discovery and development. It further addresses troubleshooting and optimization strategies for analytical and regulatory challenges and concludes with validation frameworks and a comparative analysis of global regulatory landscapes. This guide synthesizes technical and regulatory knowledge essential for innovating within the modern, data-driven pharmaceutical ecosystem.
Understanding Coordination Environments: From Molecular Networks to System-Level Regulation
In pharmaceutical science, coordination describes specific, structured interactions between a central molecule and surrounding entities, dictating the behavior and efficacy of therapeutic agents. This concept extends from the atomic level, where metal ions form coordination complexes with organic ligands, to macroscopic biological networks involving drug-receptor interactions and cellular signaling pathways. The coordination environment—the specific arrangement and identity of atoms, ions, or molecules directly interacting with a central entity—is a critical determinant of a drug's physicochemical properties, biological activity, and metabolic fate [1] [2]. Understanding and manipulating these environments allows researchers to enhance drug solubility, modulate therapeutic activity, reduce toxicity, and overcome biological barriers, making coordination a fundamental principle in modern drug design and development [3] [4].
The study of coordination in pharmaceuticals bridges traditional inorganic chemistry with contemporary molecular biology. Historically, the field was dominated by metal-based drugs like cisplatin, a platinum coordination complex that cross-links DNA to exert its anticancer effects [2]. Today, the scope has expanded to include organic coordination systems such as deep eutectic solvents (DES) for solubility enhancement and sophisticated computational models that predict how drugs coordinate with biological targets [3] [5]. This guide provides a comparative analysis of these diverse coordination systems, detailing their underlying mechanisms, experimental characterization techniques, and applications in the pharmaceutical industry, framed within the broader context of coordination environment analysis research.
Comparative Analysis of Coordination-Based Pharmaceutical Systems
The table below objectively compares three primary coordination systems used in pharmaceutical research and development, summarizing their core coordination chemistry, key performance parameters, and primary applications.
Table 1: Performance Comparison of Coordination-Based Pharmaceutical Systems
| System Type | Core Coordination Chemistry | Key Performance Parameters | Reported Efficacy/Data | Primary Pharmaceutical Applications |
|---|---|---|---|---|
| Metal-Drug Complexes [1] [2] [4] | Coordinate Covalent Bonding: Central metal ion (e.g., Pt, Cu, Au, Zn) bound to electron-donating atoms in organic ligand pharmaceuticals. | - Cytotoxic Activity (IC50)- DNA Binding Affinity- Thermodynamic Stability Constant | - Cisplatin: Potent cytotoxicity against head/neck tumors [2].- [Au(TPP)]Cl complex: Significant in-vitro/in-vivo anti-cancer activity [2].- Cu(PZA)₂Cl₂: 1:2 (Metal:Ligand) coordination confirmed [1]. | |
| Deep Eutectic Solvents (DES) [3] | Hydrogen Bonding: A hydrogen bond donor (HBD) and acceptor (HBA) form a mixture with a melting point lower than its individual components. | - Solubility Enhancement- Dissolution Kinetics- Thermodynamic Model Fit (e.g., UNIQUAC) | - TBPB:DEG DES increased solubility of Ibuprofen & Empagliflozin [3].- Dissolution was endothermic, increasing with temperature/DES concentration [3].- UNIQUAC model provided the most accurate correlation [3]. | |
| AI-Modeled Drug-Target Interactions [5] [6] | Non-covalent & Covalent Docking: Computational prediction of binding poses and energies via hydrogen bonding, van der Waals, electrostatic, and hydrophobic interactions. | - Binding Free Energy (ΔG, kcal/mol)- Predictive Accuracy vs. Experimental Data- Virtual Screening Enrichment | - Schrödinger's GlideScore: Maximizes separation of strong vs. weak binders [5].- DeepMirror AI: Speeds up drug discovery by up to 6x, reduces ADMET liabilities [5].- AI facilitates de novo molecular design [6]. |
Experimental Protocols for Analyzing Coordination Systems
Protocol 1: Solubility Enhancement with Deep Eutectic Solvents
This protocol outlines the experimental methodology for determining the solubility of poorly water-soluble drugs in aqueous Deep Eutectic Solvent (DES) systems, as derived from recent research [3].
- Objective: To measure the apparent equilibrium solubility and dissolution kinetics of active pharmaceutical ingredients (APIs) in DES-water mixtures and to correlate the data with thermodynamic models.
- Materials:
- API Model Compounds: Ibuprofen (IBU) and Empagliflozin (EMPA).
- DES Synthesis: Tetrabutylphosphonium bromide (TBPB) as hydrogen bond acceptor (HBA) and diethylene glycol (DEG) as hydrogen bond donor (HBD), combined at a specific molar ratio.
- Solvent: Deionized water for preparing aqueous DES mixtures.
- Methodology:
- DES Synthesis & Characterization: Synthesize the DES by mixing TBPB and DEG under specific conditions. Confirm the formation of the eutectic mixture using techniques like Fourier-Transform Infrared (FTIR) spectroscopy to observe hydrogen bond formation.
- Preparation of Aqueous DES Systems: Prepare eleven different mass fractions of the synthesized DES in water to create a range of solvent environments with varying polarities.
- Solubility Measurement: Add an excess amount of the API (IBU or EMPA) to each DES-water mixture. Equilibrate the suspensions in an incubator shaker at controlled temperatures (e.g., 20°C, 30°C, 40°C) for 24 hours to ensure equilibrium is reached.
- Sampling & Analysis: After equilibration, separate the supernatant from undissolved solids by filtration. Analyze the concentration of the dissolved API in the supernatant using a validated analytical method, such as High-Performance Liquid Chromatography (HPLC) with UV detection.
- Dissolution Kinetics: Monitor the dissolution profile over time (up to 24 hours) to differentiate between true equilibrium solubility and metastable supersaturated states.
- Data Correlation: Fit the experimental solubility data to thermodynamic models (Wilson, NRTL, UNIQUAC) using regression analysis to determine the model parameters and assess which model provides the best correlation.
- Key Findings: The study found that solubility for both drugs increased with rising temperature and DES concentration, indicating an endothermic dissolution process. Ibuprofen generally achieved higher dissolution than empagliflozin in the TBPB:DEG DES-water system. Among the models, UNIQUAC provided the most accurate correlation with the experimental data [3].
Protocol 2: Synthesis and Characterization of a Metal-Drug Complex
This protocol details the synthesis and physicochemical characterization of a coordination complex between a metal ion and a pharmaceutical ligand, using a Pyrazinamide (PZA)-Copper complex as an example [1].
- Objective: To synthesize a metal-drug coordination complex and characterize its structure, composition, and morphology.
- Materials:
- Pharmaceutical Ligand: Pyrazinamide (PZA).
- Metal Salt: Copper(II) chloride dihydrate (CuCl₂·2H₂O).
- Solvents: Suitable solvents for synthesis and purification (e.g., water, ethanol).
- Methodology:
- Synthesis: Dissolve the PZA ligand in a warm solvent. Slowly add an aqueous solution of the copper salt under constant stirring. Maintain the reaction mixture at a specific temperature and pH to facilitate complex formation. The resulting solid complex is isolated by filtration, washed thoroughly, and dried.
- Elemental Analysis (EA): Determine the elemental composition (C, H, N, S, metal content) of the complex. This data is used to confirm the Metal:Ligand (Me:L) ratio, which was found to be 1:2 for [Cu(PZA)₂]Cl₂ [1].
- Spectroscopic Characterization:
- FTIR Spectroscopy: Analyze the ligand and the complex. A shift in the vibrational frequencies of key functional groups (e.g., -C=O stretch, ring nitrogen vibrations) upon complexation indicates coordination through those atoms [1].
- Mass Spectrometry (MS): Use MS to confirm the molecular weight of the complex and identify fragments, which helps verify the proposed structure [1].
- Morphological Analysis:
- Scanning Electron Microscopy (SEM): Image the complex to analyze its particle size, shape, and surface topography. The [Cu(PZA)₂]Cl₂ complex showed acicular (needle-like) particles with an average size of about 1.5 microns [1].
- Energy-Dispersive X-ray Spectroscopy (EDS): Coupled with SEM, EDS is used to detect and map the elemental composition (e.g., Cu, Cl) within the synthesized complex, confirming the presence of the metal in the sample [1].
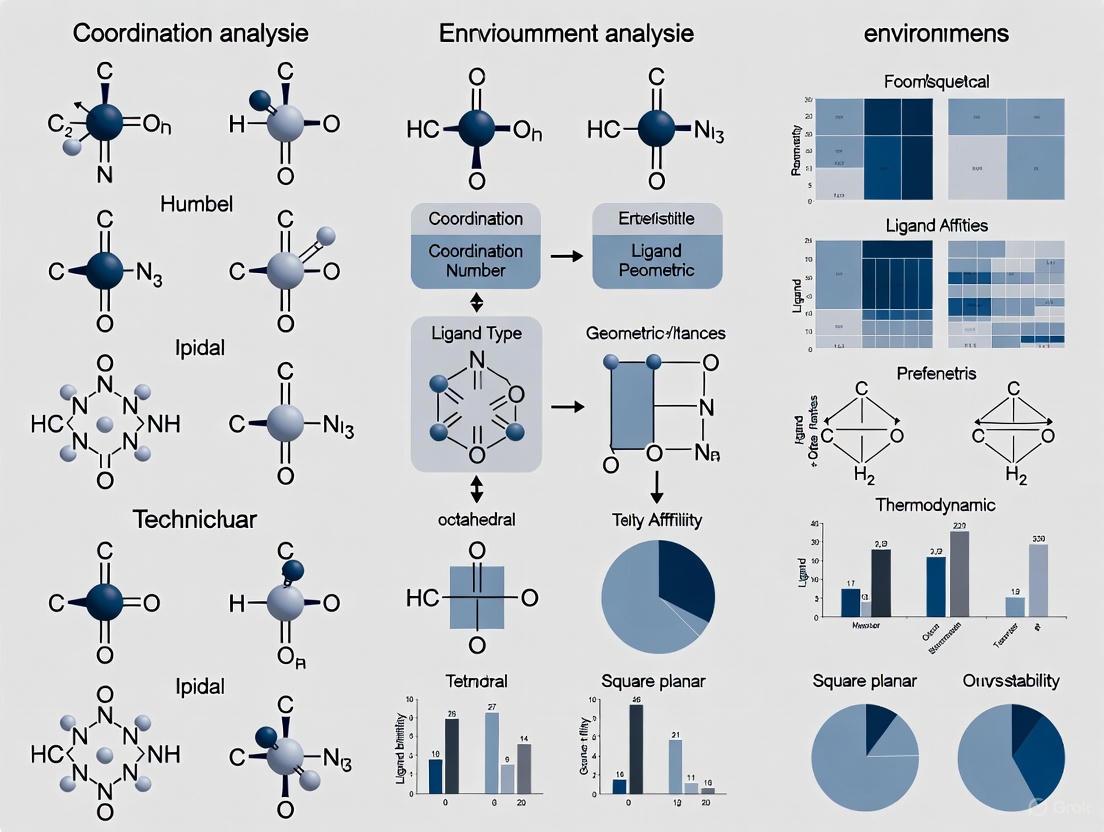
Diagram 1: Metal-Drug Complex Characterization Workflow
The Scientist's Toolkit: Key Reagents & Materials
Successful research into pharmaceutical coordination environments relies on a suite of specialized reagents, software, and analytical instruments. The following table details the essential components of the modern scientist's toolkit in this field.
Table 2: Essential Research Reagent Solutions for Coordination Environment Analysis
| Tool Name/ Category | Function in Coordination Analysis | Specific Role in Pharmaceutical Development |
|---|---|---|
| Deep Eutectic Solvents (DES) [3] | Serves as a tunable solvent medium whose components can coordinate with APIs. | Enhances the solubility and dissolution of poorly water-soluble drugs (e.g., Ibuprofen) by forming a coordinated network around the drug molecule. |
| Biogenic Metal Salts (e.g., Cu, Zn, Fe, Co) [2] [4] | Act as the central ion for forming coordination complexes with drug ligands. | Used to synthesize metal-based drugs to improve efficacy, alter pharmacological profiles, or provide novel mechanisms of action (e.g., cytotoxic agents). |
| Schrödinger Software Suite [5] | Provides computational modeling of coordination and binding environments. | Predicts binding affinity and pose of a drug candidate coordinating with a protein target using methods like Free Energy Perturbation (FEP). |
| Chemical Computing Group MOE [5] | A comprehensive platform for molecular modeling and simulation. | Facilitates structure-based drug design, molecular docking, and QSAR modeling to study and predict drug-target coordination. |
| FTIR Spectrometer [1] | Characterizes molecular vibrations to identify functional groups involved in coordination. | Detects shifts in vibrational peaks (e.g., C=O, N-H) to confirm the atoms of a drug ligand involved in binding to a metal ion. |
| Scanning Electron Microscope (SEM) [1] | Images the surface morphology and particle size of solid materials. | Reveals the physical form (e.g., crystals, amorphous aggregates) of synthesized metal-drug complexes or API particles after processing. |
Visualization of Coordination Pathways and Workflows
Coordination in Drug Action: From Metal Complex to Therapeutic Effect
The therapeutic action of metal-based drugs involves a critical coordination-driven pathway. The diagram below illustrates the multi-step mechanism of how a metal-drug complex, such as a platinum or gold complex, exerts its cytotoxic effect.
Diagram 2: Metal-Drug Complex Therapeutic Pathway
Integrated Workflow for AI-Guided Drug Coordination Design
The application of Artificial Intelligence (AI) has revolutionized the design of molecules with optimized coordination properties. This workflow charts the integrated computational and experimental cycle for AI-guided drug design, from initial data processing to lead optimization.
Diagram 3: AI-Guided Drug Design Workflow
The comparative analysis presented in this guide underscores that coordination is a unifying principle across diverse pharmaceutical disciplines, from enhancing drug solubility with Deep Eutectic Solvents to designing novel metal-based chemotherapeutics and predicting drug-target interactions with AI. The choice of coordination system is not a matter of superiority but of strategic application, dictated by the specific pharmaceutical challenge. Metal complexes offer unique mechanisms of action, DES provide a tunable platform for formulation, and AI models deliver predictive power for rapid optimization.
The future of coordination in pharmaceuticals lies in the intelligent integration of these systems. The experimental protocols and toolkits detailed herein provide a foundation for researchers to manipulate coordination environments deliberately. As characterization techniques become more advanced and computational models more accurate, the precision with which we can engineer these interactions will only increase. This will inevitably lead to a new generation of therapeutics with enhanced efficacy, reduced side effects, and tailored biological fates, solidifying the role of coordination environment analysis as a cornerstone of modern drug development.
The Role of Network Analysis in Mapping Drug-Target Interactions and Multiscale Mechanisms
Network analysis has emerged as a transformative approach in pharmacology, enabling researchers to move beyond the traditional "one drug, one target" paradigm to a more comprehensive understanding of drug action within complex biological systems. Systems pharmacology represents an evolution in this field, using computational and experimental systems biology approaches to expand network analyses across multiple scales of biological organization, explaining both therapeutic and adverse effects of drugs [7]. This methodology stands in stark contrast to earlier black-box approaches that treated cellular and tissue-level systems as opaque, often leading to confounding situations during drug discovery when promising cell-based assays failed to translate to in vivo efficacy or produced unpredictable adverse events [7].
The fundamental principle of network analysis in pharmacology involves representing biological entities as nodes (such as genes, proteins, drugs, and diseases) and their interactions as edges (including protein-protein interactions, drug-target interactions, or transcriptional regulation) [7]. This network perspective allows researchers to explicitly track drug effects from atomic-level interactions to organismal physiology, creating explicit relationships between different scales of organization—from molecular and cellular levels to tissue, organ, and ultimately organismal levels [7]. The application of network analysis in pharmacology has become increasingly crucial as we recognize that most complex diseases involve perturbations to multiple biological pathways and networks rather than single molecular defects.
Comparative Analysis of Network-Based Methodologies
Network-based approaches for mapping drug-target interactions (DTIs) can be broadly categorized into several methodological frameworks, each with distinct strengths, limitations, and optimal use cases. The current landscape is dominated by three primary approaches: ligand similarity-based methods, structure-based methods, and heterogeneous network models [8]. Each methodology offers different capabilities for predicting drug-target interactions, with varying requirements for structural data, computational resources, and ability to integrate multiscale biological information.
Table 1: Comparison of Network-Based Methodologies for DTI Prediction
| Methodology | Key Features | Data Requirements | Strengths | Limitations |
|---|---|---|---|---|
| Ligand Similarity-Based Methods (e.g., DTiGEMS, Similarity-based CNN) | Compares drug structural similarity using SMILES or molecular fingerprints [8] | Drug chemical structures, known DTIs | Computationally efficient; leverages chemical similarity principles [8] | Overlooks dynamic interactions and complex spatial structures; assumes structurally similar drugs share targets [8] |
| Structure-Based Methods (e.g., DeepDTA, DeepDrug3D) | Uses molecular docking and 3D structural information of proteins and drugs [8] | 3D structures of targets and ligands; binding affinity data | Provides mechanistic insights into binding interactions; high accuracy when structural data available [8] | Limited to proteins with known structures; computationally intensive; requires high-quality binding data [8] |
| Heterogeneous Network Models (e.g., MVPA-DTI, iGRLDTI) | Integrates multisource data (drugs, proteins, diseases, side effects) into unified network [8] | Multiple biological data types (sequence, interaction, phenotypic) | Captures higher-order relationships; works with sparse data; integrates biological context [8] | Complex model architecture; requires careful integration of heterogeneous data sources [8] |
| Large Language Model Applications (e.g., MolBERT, ProtT5) | Applies protein-specific LLMs to extract features from sequences [8] | Protein sequences, drug molecular representations | Does not require 3D structures; captures functional relevance from sequences; generalizes well [8] | Limited direct structural insights; dependent on pretraining data quality and coverage [8] |
Performance Comparison of DTI Prediction Methods
Quantitative evaluation of network-based DTI prediction methods reveals significant differences in performance metrics across benchmark datasets. The integration of multiple data types and advanced neural network architectures in recent heterogeneous network models has demonstrated superior performance compared to traditional approaches.
Table 2: Experimental Performance Metrics of DTI Prediction Methods
| Method | AUROC | AUPR | Accuracy | F1-Score | Key Innovations |
|---|---|---|---|---|---|
| MVPA-DTI (Proposed) | 0.966 [8] | 0.901 [8] | - | - | Multiview path aggregation; molecular attention transformer; Prot-T5 integration [8] |
| iGRLDTI | - | - | - | - | Edge weight regulation; regularization in GNN [8] |
| DTiGEMS+ | - | - | - | - | Similarity selection and fusion algorithm [8] |
| Similarity-based CNN | - | - | - | - | Outer product of similarity matrix; 2D CNN [8] |
| DeepDTA | - | - | - | - | Incorporates 3D structural information [8] |
The MVPA-DTI model demonstrates state-of-the-art performance, showing improvements of 1.7% in AUPR and 0.8% in AUROC over baseline methods [8]. This performance advantage stems from its ability to integrate multiple views of biological data, including drug structural information, protein sequence features, and heterogeneous network relationships.
Experimental Protocols and Workflows
MVPA-DTI Workflow Implementation
The MVPA-DTI (Multiview Path Aggregation for Drug-Target Interaction) framework implements a comprehensive workflow for predicting drug-target interactions through four major phases: multiview feature extraction, heterogeneous network construction, meta-path aggregation, and interaction prediction [8]. The following diagram illustrates the complete experimental workflow:
Protocol Details: Multiview Feature Extraction
Drug Structural Feature Extraction Protocol: The molecular attention transformer processes drug chemical structures to extract 3D conformational features through a physics-informed attention mechanism [8]. This approach begins with molecular graph representations, where atoms are represented as nodes and bonds as edges. The transformer architecture incorporates spatial distance matrices and quantum chemical properties to compute attention weights that reflect both structural and electronic characteristics of drug molecules. The output is a continuous vector representation that encodes the three-dimensional structural information critical for understanding binding interactions.
Protein Sequence Feature Extraction Protocol: The Prot-T5 model, a protein-specific large language model, processes protein sequences to extract biophysically and functionally relevant features [8]. The protocol involves feeding amino acid sequences through the pretrained transformer architecture, which has been trained on massive protein sequence databases to understand evolutionary patterns and structural constraints. The model generates contextual embeddings for each residue and global protein representations that capture functional domains, binding sites, and structural motifs without requiring explicit 3D structural information.
Protocol Details: Heterogeneous Network Construction
The heterogeneous network integrates multiple biological entities including drugs, proteins, diseases, and side effects from multisource databases [8]. The construction protocol involves:
- Node Identification: Define nodes for each entity type with unique identifiers and metadata annotations.
- Edge Establishment: Create edges based on known interactions (drug-target, drug-disease, target-disease) and similarity metrics (drug-drug similarity, target-target similarity).
- Feature Assignment: Assign the extracted drug and protein features to corresponding nodes.
- Network Validation: Verify connectivity and biological relevance through cross-referencing with established biological databases.
This constructed network serves as the foundation for the meta-path aggregation mechanism that captures higher-order relationships between biological entities.
Research Reagents and Computational Tools
The implementation of advanced network analysis methods for drug-target interaction prediction requires specialized computational tools and biological resources. The following table details essential research reagents and solutions used in the featured methodologies.
Table 3: Research Reagent Solutions for Network Analysis in DTI Prediction
| Resource Category | Specific Tools/Databases | Function | Application Context |
|---|---|---|---|
| Protein Language Models | Prot-T5, ProtBERT, TAPE [8] | Extract features from protein sequences; capture functional relevance without 3D structures [8] | Feature extraction from protein sequences; transfer learning for DTI prediction [8] |
| Molecular Representation | Molecular Attention Transformer, MolBERT, ChemBERTa [8] | Process drug chemical structures; generate molecular embeddings [8] | Drug feature extraction; molecular property prediction [8] |
| Graph Neural Networks | Regulation-aware GNN, Meta-path Aggregation frameworks [8] | Model heterogeneous biological networks; learn node representations [8] | Heterogeneous network construction; relationship learning between biological entities [8] |
| Interaction Databases | DrugBank, KEGG, STRING, BioGRID | Provide known DTIs; protein-protein interactions; pathway information | Ground truth data for model training; biological validation [7] [8] |
| Omics Technologies | Genomic sequencing; Transcriptomic profiling; Proteomic assays [7] | Generate systems-level data on drug responses; identify genetic variants affecting drug efficacy [7] | Multiscale mechanism analysis; personalized therapy development [7] |
| Evaluation Frameworks | AUROC/AUPR calculation; Cross-validation; Case study protocols [8] | Quantitative performance assessment; real-world validation [8] | Method comparison; practical utility assessment [8] |
Case Study: KCNH2 Target Application
A concrete application of the MVPA-DTI framework demonstrates its practical utility in drug discovery. For the voltage-gated inward-rectifying potassium channel KCNH2—a target relevant to cardiovascular diseases—the model was employed for candidate drug screening [8]. Among 53 candidate drugs, MVPA-DTI successfully predicted 38 as having interactions with KCNH2, with 10 of these already validated in clinical treatment [8]. This case study illustrates how network analysis approaches can significantly accelerate drug repositioning efforts by prioritizing candidates with higher probability of therapeutic efficacy.
The following diagram illustrates the network relationships and prediction workflow for the KCNH2 case study:
This case study exemplifies how heterogeneous network analysis successfully integrates multiple data types—including known drug interactions, disease associations, and protein interaction partners—to generate clinically relevant predictions for drug repositioning.
Network analysis has fundamentally transformed our approach to mapping drug-target interactions and understanding multiscale mechanisms of drug action. The progression from simple ligand-based similarity methods to sophisticated heterogeneous network models that integrate multiview biological data represents a paradigm shift in pharmacological research [7] [8]. These approaches have demonstrated superior performance in predicting drug-target interactions while providing insights into the complex network relationships that underlie both therapeutic efficacy and adverse effects.
The future of network analysis in pharmacology will likely focus on several key areas: (1) enhanced integration of multiscale data from genomics, proteomics, and metabolomics; (2) development of more interpretable models that provide mechanistic insights alongside predictive accuracy; (3) application to personalized medicine through incorporation of individual genomic variation; and (4) expansion to model dynamic network responses to drug perturbations over time [7]. As these methodologies continue to evolve, they will increasingly enable the prediction of therapeutic efficacy and adverse event risk for individuals prior to commencement of therapy, ultimately fulfilling the promise of personalized precision medicine [7].
Systems pharmacology represents a paradigm shift in pharmacology, applying computational and experimental systems biology approaches to the study of drugs, drug targets, and drug effects [9] [10]. This framework moves beyond the traditional "one drug, one target" model to consider drug actions within the complex network of biological systems, enabling a more comprehensive analysis of both therapeutic and adverse effects [11]. By studying drugs in the context of cellular networks, systems pharmacology provides insights into adverse events caused by off-target drug interactions and complex network responses, allowing for rapid identification of biomarkers for side effect susceptibility [9].
The approach integrates large-scale experimental studies with computational analyses, focusing on the functional interactions within biological networks rather than single transduction pathways [11]. This network perspective is particularly valuable for understanding complex patterns of drug action, including synergy and oscillatory behavior, as well as disease progression processes such as episodic disorders [11]. The ultimate goal of systems pharmacology is to develop not only more effective therapies but also safer medications with fewer side effects through predictive modeling of therapeutic efficacy and adverse event risk [9] [10].
Methodological Framework and Comparison with Alternative Approaches
Core Principles of Systems Pharmacology
Systems pharmacology employs mechanistically oriented modeling that integrates drug exposure, target biology, and downstream effectors across molecular, cellular, and pathophysiological levels [12]. These models characterize fundamental properties of biological systems behavior, including hysteresis, non-linearity, variability, interdependency, convergence, resilience, and multi-stationarity [11]. The framework is particularly useful for describing effects of multi-target interactions and homeostatic feedback on pharmacological response, distinguishing symptomatic from disease-modifying effects, and predicting long-term impacts on disease progression from short-term biomarker responses [11].
Quantitative Systems Pharmacology (QSP), a specialized form of this approach, has demonstrated significant impact across the drug development continuum [12]. QSP models integrate drug disposition characteristics, target binding kinetics, and transduction dynamics to create a common drug-exposure and disease "denominator" for performing quantitative comparisons [12]. This enables researchers to compare compounds of interest against later-stage development candidates or marketed products, evaluate different therapeutic modalities for a given target, and optimize dosing regimens based on simulated efficacy and safety metrics [12].
Comparative Analysis with Other Pharmacological Methods
Systems pharmacology differs fundamentally from traditional pharmacological approaches and other modern techniques in its theoretical foundation and application. The table below provides a structured comparison of these methodologies:
Table 1: Comparison of Systems Pharmacology with Alternative Methodological Approaches
| Methodology | Theoretical Foundation | Application Scope | Data Requirements | Key Advantages | Principal Limitations |
|---|---|---|---|---|---|
| Systems Pharmacology | Network analysis of biological systems; computational modeling of drug-target interactions [9] | Prediction of therapeutic and adverse effects through network context [9] [11] | Large-scale experimental data, network databases, computational resources [10] | Identifies multi-scale mechanisms; predicts network-level effects [10]; enables target identification and polypharmacology [9] | Complex model development; requires multidisciplinary expertise; computational intensity |
| Gene Chip Technology | Experimental high-throughput screening; microarray hybridization of known gene sequences [13] | Target prediction through experimental measurement of gene expression changes | Gene chips, laboratory equipment for RNA processing and hybridization | Direct experimental measurement; does not require prior published data | Higher cost; longer time requirements; experimental variability [13] |
| Traditional PK/PD Modeling | Physiology-based pharmacokinetic and pharmacodynamic models with linear transduction pathways [11] | Characterization of drug disposition and effect relationships using simplified pathways | Clinical PK/PD data, drug concentration measurements | Established regulatory acceptance; simpler mathematical framework | Fails to explain complex network interactions; limited prediction of adverse events [11] |
| Quantitative Systems Pharmacology (QSP) | Mechanistic modeling connecting drug targets to clinical endpoints across biological hierarchies [12] [14] | Dose selection and optimization; safety differentiation; combination therapy decisions [12] [14] | Systems biology data, omics technologies, knowledge bases, clinical endpoints [12] | Supports regulatory submissions; enables virtual patient populations; predicts long-term outcomes [14] | High resource investment; model qualification challenges; specialized expertise required |
Experimental Evidence: Direct Comparison Study
A 2022 comparative study directly evaluated the performance of systems pharmacology against gene chip technology for predicting targets of ZhenzhuXiaojiTang (ZZXJT), a traditional Chinese medicine formula for primary liver cancer [13]. The research provided quantitative experimental data on the relative performance of these approaches:
Table 2: Experimental Comparison of Target Prediction Performance Between Systems Pharmacology and Gene Chip Technology
| Performance Metric | Systems Pharmacology | Gene Chip Technology |
|---|---|---|
| Identified Target Rate | 17% of predicted targets | 19% of predicted targets |
| Molecular Docking Performance | Top ten targets demonstrated better binding free energies | Inferior binding free energies compared to systems pharmacology |
| Core Drug Prediction Consistency | High consistency with experimental results | High consistency with experimental results |
| Core Small Molecule Prediction | Moderate consistency | Moderate consistency |
| Methodological Advantages | Cost-effective; time-efficient; leverages existing research data [13] | Direct experimental measurement; no prior data requirement |
| Methodological Limitations | Dependent on quality of existing databases | Higher cost; longer experimental duration; technical variability |
This experimental comparison demonstrated that while gene chip technology identified a slightly higher percentage of targets (19% vs. 17%), the systems pharmacology approach predicted targets with superior binding energies in molecular docking studies, suggesting higher quality predictions [13]. Furthermore, systems pharmacology achieved these results with significantly reduced cost and time requirements, highlighting its efficiency advantages for initial target screening and hypothesis generation [13].
Experimental Protocols and Methodologies
Standardized Workflow for Systems Pharmacology Analysis
The implementation of systems pharmacology follows a structured workflow that ensures reproducible development and qualification of models. This workflow encompasses data programming, model development, parameter estimation, and qualification [12]. The progressive maturation of this workflow represents a necessary step for efficient, reproducible development of QSP models, which are inherently iterative and evolutive [12].
Table 3: Core Components of a Standardized Systems Pharmacology Workflow
| Workflow Component | Key Features | Implementation Tools |
|---|---|---|
| Data Programming | Conversion of raw data to standard format; creation of master dataset for exploration [12] | Common data format for QSP and population modeling; automated data processing |
| Model Development | Multiconditional model setup; handling of heterogeneous datasets; flexible model structures [12] | Ordinary differential equations; possible agent-based or partial differential equation components |
| Parameter Estimation | Multistart strategy for robust optimization; assessment of parameter identifiability [12] | Profile likelihood method; Fisher information matrix; confidence interval computation |
| Model Qualification | Evaluation of model performance across experimental conditions; assessment of predictive capability [12] | Visual predictive checks; benchmarking against experimental data; sensitivity analysis |
Detailed Protocol for Network-Based Target Identification
The following experimental protocol outlines the standard methodology for identifying drug targets using systems pharmacology, as applied in the ZZXJT case study [13]:
Screening of Active Ingredients and Targets
- Source active ingredients from relevant databases (e.g., Traditional Chinese Medicine Systems Pharmacology Database - TCMSP)
- Apply ADME-based screening criteria (Oral Bioavailability ≥ 30%; Drug-likeness ≥ 0.18)
- Remove ingredients without known targets and integrate target protein information
- Normalize target information using standardized protein databases (UniProt)
Disease Target Identification
- Mine disease-related targets from specialized databases (OMIM, GeneCards)
- Apply relevance score filtering (e.g., GeneCards relevance score ≥ 15)
- Merge data from multiple sources to create comprehensive disease target dataset
Network Construction and Analysis
- Identify intersecting targets between drug and disease using Venn diagrams
- Submit intersecting targets to interaction databases (STRING) to construct Protein-Protein Interaction (PPI) networks
- Set appropriate confidence levels (≥ 0.4) and organism parameters (Homo sapiens)
- Import networks to visualization software (Cytoscape) and analyze core potential proteins by "combined degree" values
Gene Enrichment Analysis
- Perform pathway analysis using specialized databases (Metascape)
- Conduct Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis
- Execute Gene Ontology (GO) analysis across three categories: Biological Process (BP), Cellular Component (CC), and Molecular Function (MF)
- Apply appropriate statistical thresholds (p < 0.01) and display results using data visualization tools
Experimental Validation through Molecular Docking
To validate predictions from systems pharmacology, molecular docking serves as a critical experimental confirmation step [13]. The protocol includes:
- Preparation of Predicted Targets: Select top target proteins from systems pharmacology predictions
- Ligand Preparation: Generate 3D structures of active compounds identified through systems pharmacology screening
- Docking Simulation: Perform computational docking studies to evaluate binding interactions and calculate binding free energies
- Benchmark Comparison: Compare docking results with positive control targets to assess relative performance against alternative prediction methods
This validation approach demonstrated that systems pharmacology predictions had superior binding free energies compared to gene chip-based predictions, confirming the method's value for identifying high-quality targets [13].
Visualization of Systems Pharmacology Framework
The following diagram illustrates the core workflow and network interactions in systems pharmacology, highlighting the integration of data sources, computational modeling, and outcome prediction:
Figure 1: Systems Pharmacology Workflow Integrating Multiscale Data for Therapeutic and Adverse Effect Prediction
Implementation of systems pharmacology requires specialized databases, software tools, and computational resources. The following table catalogs essential research reagents and solutions for conducting systems pharmacology research:
Table 4: Essential Research Resources for Systems Pharmacology Investigations
| Resource Category | Specific Tools/Databases | Primary Function | Application Context |
|---|---|---|---|
| Compound Databases | TCMSP (Traditional Chinese Medicine Systems Pharmacology Database) [13] | Active ingredient identification and ADME screening | Initial compound screening for natural products and traditional medicines |
| Target Databases | UniProt Protein Database [13] | Protein target normalization and standardization | Unified target information across multiple data sources |
| Disease Target Resources | OMIM, GeneCards [13] | Disease-related target mining and prioritization | Identification of pathological mechanisms and potential therapeutic targets |
| Network Analysis Tools | STRING Database [13] | Protein-protein interaction network construction | Contextualizing drug targets within cellular networks and pathways |
| Visualization Software | Cytoscape [13] | Network visualization and analysis | Identification of core network components and key targets |
| Pathway Analysis Resources | Metascape [13] | Gene enrichment analysis and functional annotation | Biological interpretation of target lists through KEGG and GO analysis |
| Molecular Docking Tools | AutoDock, Schrödinger Suite | Validation of target-compound interactions through binding energy calculations | Experimental confirmation of predicted drug-target interactions |
| QSP Modeling Platforms | MATLAB, R, Python with specialized systems biology libraries | Mathematical model development, simulation, and parameter estimation | Implementation of multiscale mechanistic models for drug and disease systems |
Regulatory Applications and Impact Assessment
The implementation of systems pharmacology, particularly Quantitative Systems Pharmacology (QSP), has demonstrated significant impact in regulatory decision-making. Landscape analysis of regulatory submissions to the US Food and Drug Administration (FDA) reveals increasing adoption of these approaches [14]. Since 2013, there has been a notable increase in QSP submissions in Investigational New Drug (IND) applications, New Drug Applications (NDAs), and Biologics License Applications (BLAs) [14].
The primary applications of QSP in regulatory contexts include dose selection and optimization, safety differentiation between drug classes, and rational selection of immuno-oncology drug combinations [12] [14]. These models provide a common framework for comparing compounds within a dynamic pathophysiological context, enabling fair comparisons between investigational drugs and established therapies [12]. The growing regulatory acceptance of QSP underscores the maturity and impact of systems pharmacology approaches in modern drug development.
QSP has proven particularly valuable in supporting efficacy and safety differentiation within drug classes, as demonstrated by applications comparing sodium-glucose cotransporter-2 (SGLT2) inhibitors for type 2 diabetes treatment [12]. Additionally, QSP models have enabled rational selection of immuno-oncology combination therapies based on efficacy projections, addressing the exponential growth in potential combination options [12]. These applications highlight how systems pharmacology frameworks facilitate more informed decision-making throughout the drug development pipeline, from early discovery to regulatory submission and post-market optimization.
The integration of artificial intelligence (AI) and machine learning (ML) is fundamentally reshaping the pharmaceutical landscape, from accelerating drug discovery to optimizing manufacturing processes. This technological shift presents both unprecedented opportunities and unique challenges for global regulators tasked with ensuring patient safety, product efficacy, and data integrity. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have emerged as pivotal forces in establishing governance for these advanced tools. While both agencies share the common goal of protecting public health, their regulatory philosophies, approaches, and technical requirements are developing with distinct characteristics. For researchers, scientists, and drug development professionals, navigating this complex and evolving regulatory environment is essential for the successful integration of AI into the medicinal product lifecycle. This guide provides a comparative analysis of the FDA and EMA frameworks, offering a foundational understanding of their current oversight structures for AI and complex data [15] [16].
Comparative Analysis of FDA and EMA Regulatory Philosophies
The FDA and EMA are spearheading the development of regulatory pathways for AI, but their approaches reflect different institutional priorities and legal traditions. The following table summarizes the core philosophical and practical differences between the two agencies.
Table 1: Core Philosophical Differences Between FDA and EMA AI Regulation
| Aspect | U.S. Food and Drug Administration (FDA) | European Medicines Agency (EMA) |
|---|---|---|
| Overall Philosophy | Pragmatic, risk-based approach under existing statutory authority [16]. | Prescriptive, control-oriented, and ethics-focused, integrated with new legislation like the AI Act [15] [16]. |
| Guiding Principle | Establishes model "credibility" for a specific "Context of Use (COU)" [15]. | Extends well-established Good Manufacturing Practice (GMP) principles to AI, prioritizing predictability and control [15]. |
| Scope of Initial Guidance | Broad, covering the entire product lifecycle (non-clinical, clinical, manufacturing) where AI supports regulatory decisions [17] [15]. | Narrower and more deliberate, initially focused on "critical applications" in manufacturing via GMP Annex 22 [15]. |
| Approach to Model Adaptivity | Accommodates adaptive AI through a "Life Cycle Maintenance Plan," creating a pathway for continuous learning [15]. | Restrictive; proposed GMP Annex 22 prohibits adaptive models in critical processes, allowing only static, deterministic models [15]. |
| Primary Regulatory Tool | Draft guidance: "Considerations for the Use of Artificial Intelligence..." (Jan 2025) [17] [15]. | Reflection paper (2024); proposed GMP Annex 22 on AI; EU AI Act [18] [15] [19]. |
The FDA's strategy is characterized by flexibility. Its central doctrine is the "Context of Use (COU)", which means the agency evaluates the trustworthiness of an AI model for a specific, well-defined task within the drug development pipeline. This allows for a nuanced, risk-based assessment rather than a one-size-fits-all rule. The FDA's choice of the term "credibility" over the traditional "validation" is significant, as it acknowledges the probabilistic nature of AI systems and allows for acceptance if the COU includes appropriate risk mitigations [15].
In contrast, the EMA's approach, particularly for manufacturing, is deeply rooted in the established principles of GMP: control, predictability, and validation. The proposed GMP Annex 22 seeks to integrate AI into this existing framework rather than create a entirely new paradigm. This results in a more restrictive and prescriptive stance, especially regarding the types of AI models permitted. The Annex explicitly mandates the use of only static and deterministic models in critical GMP applications, effectively prohibiting continuously learning AI, generative AI, and Large Language Models (LLMs) in these settings due to their inherent variability [15].
The following diagram illustrates the high-level logical progression of the two regulatory pathways, from development to ongoing oversight.
Detailed Framework Requirements and Experimental Protocols
For researchers, understanding the specific technical and documentation requirements is crucial for compliance. Both regulators demand rigorous evidence of an AI model's safety, performance, and robustness, though the nature of this evidence differs.
The FDA's Credibility Assessment Framework
The FDA's draft guidance outlines a multi-step, risk-based framework for establishing and documenting an AI model's credibility for its intended COU [15]. The agency's assessment of risk is a function of "model influence" (how much the output drives a decision) and "decision consequence" (the impact of an incorrect decision on patient health or product quality) [15].
Table 2: Key Phases of the FDA's AI Model Credibility Assessment
| Phase | Core Objective | Key Documentation & Experimental Protocol |
|---|---|---|
| 1. Definition | Precisely define the question the AI model will address and its specific Context of Use (COU). | A detailed COU specification document describing the model's purpose, operating environment, and how outputs inform decisions [15]. |
| 2. Risk Assessment | Evaluate the model's risk level based on its influence and the consequence of an error. | A risk assessment report classifying the model as low, medium, or high risk, justifying the classification with a defined risk matrix [15]. |
| 3. Planning | Develop a tailored Credibility Assessment Plan to demonstrate trustworthiness for the COU. | A comprehensive plan detailing data management strategies, model architecture, feature selection, and evaluation methods using independent test data [15] [20]. |
| 4. Execution & Monitoring | Execute the plan and ensure ongoing performance through the product lifecycle. | Model validation reports, performance metrics on test data, and a Life Cycle Maintenance Plan for monitoring and managing updates [15]. |
A critical component of the FDA's framework is the Life Cycle Maintenance Plan. This plan acts as a regulatory gateway for adaptive AI systems, requiring sponsors to outline [15]:
- Performance monitoring metrics and frequency
- Triggers for model re-testing or re-validation
- Procedures for managing and documenting model updates
The EMA's Principles for AI in the Medicinal Product Lifecycle
The EMA's approach, detailed in its reflection paper and supported by the network's AI workplan, emphasizes a human-centric approach where AI use must comply with existing legal frameworks and ethical standards [18] [19]. For manufacturing specifically, the proposed GMP Annex 22 is highly prescriptive.
Table 3: Core Requirements under EMA's Proposed GMP Annex 22 for AI
| Requirement Category | EMA Expectation & Protocol |
|---|---|
| Model Type & Explainability | Only static, deterministic models are permitted for critical applications. "Black box" models are unacceptable; models must be explainable, and outputs should include confidence scores for human review [15]. |
| Data Integrity & Testing | Test data must be completely independent of training data, representative of full process variation, and accurately labeled by subject matter experts. Use of synthetic data is discouraged [15]. |
| Human Oversight & Accountability | Formalized "Human-in-the-Loop" (HITL) oversight is required. Ultimate responsibility for GMP decisions rests with qualified personnel, not the algorithm [15]. |
| Change Control | Deployed models are under strict change control. Any modification to the model, system, or input data sources requires formal re-evaluation [15]. |
The following workflow diagram synthesizes the core experimental and validation protocols that researchers should embed into their AI development process to meet regulatory expectations.
The Scientist's Toolkit: Essential Research Reagents for AI Regulation
For scientists and developers building AI solutions for the regulated pharmaceutical space, the following "reagents" or core components are essential for a successful regulatory submission.
Table 4: Essential Components for AI Research and Regulatory Compliance
| Research Reagent | Function & Purpose in the Regulatory Context |
|---|---|
| Context of Use (COU) Document | Precisely defines the model's purpose, boundaries, and role in decision-making. This is the foundational document for any regulatory evaluation [15]. |
| Credibility Assessment Plan (FDA) | A tailored protocol detailing how the model's trustworthiness will be established for its specific COU, including data strategy, evaluation methods, and acceptance criteria [15]. |
| Independent Test Dataset | A held-out dataset, completely separate from training and tuning data, used to provide an unbiased estimate of the model's real-world performance [15] [20]. |
| Model Card | A standardized summary document included in labeling (for devices) or submission packages that communicates key model information, such as intended use, architecture, performance, and limitations [20]. |
| Bias Detection & Mitigation Framework | A set of tools and protocols used to identify, quantify, and address potential biases in the training data and model outputs to ensure fairness and generalizability [20] [21]. |
| Life Cycle Maintenance Plan | A forward-looking plan that outlines the procedures for ongoing performance monitoring, drift detection, and controlled model updates post-deployment [15]. |
The regulatory environment for AI in pharmaceuticals is dynamic and complex, with the FDA and EMA forging distinct but equally critical paths. The FDA's flexible, risk-based "credibility" framework offers a pathway for a wide array of AI applications across the drug lifecycle, including those that are adaptive. In contrast, the EMA's prescriptive, control-oriented approach, particularly in manufacturing, prioritizes stability and absolute understanding through strict model constraints. For the global research and development community, success hinges on embedding regulatory thinking into the earliest stages of AI project planning. By understanding these frameworks, implementing robust experimental and data governance protocols, and proactively engaging with regulators, scientists and drug developers can harness the power of AI to bring innovative treatments to patients safely and efficiently.
The integration of Artificial Intelligence (AI) into drug development represents a paradigm shift, offering the potential to accelerate discovery, optimize clinical trials, and personalize therapeutics. However, this promise is tempered by a complex set of challenges that form the core of this analysis. Within the framework of coordination environment analysis techniques, this guide examines three interdependent obstacles: the inherent opacity of black-box AI models, the pervasive risk of data bias, and the increasingly fragmented international regulatory landscape. The inability to fully understand, control, and standardize AI systems creates a precarious coordination environment for researchers, regulators, and industry sponsors alike. This article objectively compares the performance and characteristics of different approaches to these challenges, providing drug development professionals with a structured analysis of the current ecosystem.
The Black Box Problem: Interpretability vs. Performance
A "black box" AI describes a system where internal decision-making processes are opaque, meaning users can observe inputs and outputs but cannot discern the logic connecting them [22]. This is not an edge case but a fundamental characteristic of many advanced machine learning models, including the large language models (LLMs) and deep learning networks powering modern AI tools [23].
Comparative Analysis of AI Model Transparency
The trade-off between model performance and interpretability is a central tension in the field. The table below compares different types of AI models based on their transparency and applicability in drug development.
Table 1: Comparison of AI Model Types in Drug Development
| Model Type | Interpretability | Typical Applications in Drug Development | Key Challenges |
|---|---|---|---|
| Traditional Rule-Based AI | High (White Box) | Automated quality control, operational workflows | Limited power and flexibility for complex tasks [22] |
| Traditional Machine Learning (e.g., Logistic Regression) | High (White Box) | Preliminary patient stratification, initial data analysis | Lower predictive accuracy on complex, unstructured data [22] |
| Deep Learning/LLMs (e.g., GPT-4, Claude) | Low (Black Box) | Drug discovery, molecular behavior prediction, original content creation [22] [24] | Opacity conceals biases, vulnerabilities, and reasoning [22] [25] |
Experimental Protocols for Interpretability
Researchers are developing techniques to peer into the black box. The following experimental methodologies are central to evaluating model interpretability:
- LIME (Local Interpretable Model-agnostic Explanations): This technique creates simpler, local surrogate models that approximate the behavior of the original complex model around a specific prediction. It helps identify which input features most influenced a single decision, making the model's local behavior more understandable [25].
- SHAP (SHapley Additive exPlanations): Based on cooperative game theory, SHAP assigns each feature an "importance" value for a particular prediction. It quantifies the contribution of each feature to the difference between the actual prediction and a baseline prediction, providing a consistent and globally relevant measure of feature importance [25].
- Counterfactual (CF) Approximation Methods: These methods involve systematically modifying input data (e.g., a specific text concept) and observing changes in the model's output. This helps researchers approximate how a model's decision would change if certain factors were different, aiding in causal effect estimation [25].
The diagram below illustrates a typical experimental workflow for interpreting a black-box AI model in a research setting.
Diagram Title: Workflow for Interpreting a Black-Box AI Model
Bias in AI is a systematic and unfair discrimination that arises from flaws in data, algorithmic design, or human decision-making during development [26] [27]. In drug development, biased models can lead to skewed predictions, unequal treatment outcomes, and the perpetuation of existing health disparities.
Typology and Comparative Impact of AI Bias
Bias can infiltrate AI systems at multiple stages. The following table classifies common types of bias and their potential impact on drug development processes.
Table 2: Types of AI Bias and Their Impact in Drug Development
| Bias Type | Source | Impact Example in Drug Development |
|---|---|---|
| Data/Sampling Bias [26] [27] | Training data doesn't represent the target population. | Medical imaging algorithms for skin cancer show lower accuracy for darker skin tones if trained predominantly on lighter-skinned individuals [26]. |
| Historical Bias [26] | Past discrimination patterns are embedded in training data. | An AI model for patient recruitment might under-represent certain demographics if historical clinical trial data is non-diverse [26] [28]. |
| Algorithmic Bias [27] | Algorithm design prioritizes efficiency over fairness. | A model optimizing for trial speed might inadvertently select healthier, less diverse patients, limiting the generalizability of results. |
| Measurement Bias [26] | Inconsistent or flawed data collection methods. | Pulse oximeter algorithms overestimated blood oxygen levels in Black patients, leading to delayed treatment decisions during COVID-19 [26]. |
Experimental Protocols for Bias Mitigation
Mitigating bias requires a proactive, lifecycle approach. The experimental protocols for bias mitigation are often categorized by when they are applied:
Pre-processing Mitigation: These techniques modify the training data itself before model training. Methods include:
- Resampling: Systematically adding copies of instances from under-represented groups or removing instances from over-represented groups to create a balanced dataset [29].
- Reweighting: Assigning higher weights to instances from under-represented groups during the model training process to ensure they have a stronger influence on the learning algorithm [29].
- Disparate Impact Remover: A pre-processing algorithm that edits feature values to improve group fairness while preserving the data's utility [29].
In-processing Mitigation: These techniques modify the learning algorithm itself to incorporate fairness constraints.
- Adversarial Debiasing: An adversarial network architecture where a primary model learns to make predictions, while an adversary simultaneously tries to predict the sensitive attribute (e.g., race, gender) from the primary model's predictions. The primary model is trained to maximize predictive accuracy while minimizing the adversary's ability to predict the sensitive attribute, thus removing bias [29].
- Fairness Constraints: Incorporating mathematical fairness definitions (e.g., demographic parity, equalized odds) directly into the model's objective function as regularization terms [29].
Post-processing Mitigation: These techniques adjust the model's outputs after training.
- Threshold Adjustment: Applying different decision thresholds for different demographic groups to equalize error rates (e.g., false positive rates) [29].
- Output Calibration: Calibrating the model's probability scores for different subgroups to ensure they reflect true likelihoods equally well across groups.
The diagram below illustrates the relationship between these mitigation strategies and the machine learning lifecycle.
Diagram Title: AI Bias Mitigation Strategies in the ML Lifecycle
International Regulatory Divergence: A Comparative Analysis
As AI transforms drug development, regulatory agencies worldwide are developing frameworks to ensure safety and efficacy. However, a lack of alignment in these approaches creates significant challenges for global drug development.
Comparative Analysis of Regulatory Frameworks
The following table compares the evolving regulatory approaches to AI in drug development across major international agencies.
Table 3: Comparison of International Regulatory Approaches to AI in Drug Development
| Regulatory Agency | Key Guidance/Document | Core Approach | Notable Features |
|---|---|---|---|
| U.S. Food and Drug Administration (FDA) | "Considerations for the Use of AI to Support Regulatory Decision-Making for Drug and Biological Products" (Draft, 2025) [24] | Risk-based "Credibility Assessment Framework" centered on the "Context of Use" (COU) [24] [30]. | Focuses on the AI model's specific function and scope in addressing a regulatory question. Acknowledges challenges like data variability and model drift [24]. |
| European Medicines Agency (EMA) | "Reflection Paper on the Use of AI in the Medicinal Product Lifecycle" (2024) [24] | Structured and cautious, prioritizing rigorous upfront validation and comprehensive documentation [24]. | Issued its first qualification opinion on an AI methodology for diagnosing inflammatory liver disease in 2025, accepting AI-generated clinical trial evidence [24]. |
| UK Medicines and Healthcare products Regulatory Agency (MHRA) | "Software as a Medical Device" (SaMD) and "AI as a Medical Device" (AIaMD) principles [24] | Principles-based regulation; utilizes an "AI Airlock" regulatory sandbox to test innovative technologies [24]. | The sandbox allows for real-world testing and helps the agency identify regulatory challenges. |
| Japan's Pharmaceuticals and Medical Devices Agency (PMDA) | "Post-Approval Change Management Protocol for AI-SaMD" (2023) [24] | "Incubation function" to accelerate access; formalized process for managing post-approval AI changes. | The PACMP allows predefined, risk-mitigated modifications to AI algorithms post-approval without full resubmission, facilitating continuous improvement [24]. |
Experimental Protocol for Regulatory Compliance: The Context of Use (COU) Framework
A key experimental and documentation protocol emerging from the regulatory landscape is the FDA's Context of Use (COU) framework [24] [30]. For a researcher or sponsor, defining the COU is a critical first step in preparing an AI tool for regulatory evaluation. The protocol involves:
- Defining the Purpose: Precisely articulate the AI model's function within the drug development process (e.g., "to predict patient risk of a specific adverse event from Phase 2 clinical trial data").
- Specifying the Scope: Detail the boundaries of the model's application, including the target population, input data types, and the specific decisions or outputs it will inform.
- Linking to Regulatory Impact: Clearly state how the AI-generated information will be used to support a specific regulatory decision regarding safety, efficacy, or quality.
- Conducting a Risk-Based Credibility Assessment: Following the FDA's draft guidance, build evidence to establish trust in the model's output for the defined COU. This involves a seven-step process focusing on the model's reliability, which includes evaluating data quality, model design, and performance [24].
The Scientist's Toolkit: Research Reagent Solutions
To effectively navigate the challenges outlined, researchers require a suite of methodological and software tools. The following table details key "research reagents" for developing responsible AI in drug development.
Table 4: Essential Research Reagents for Addressing AI Challenges
| Tool/Resource | Type | Primary Function | Relevance to Challenges |
|---|---|---|---|
| LIME & SHAP [25] | Software Library | Provide local and global explanations for model predictions. | Black-Box Interpretability |
| AI Fairness 360 (AIF360) [29] | Open-Source Toolkit (IBM) | Provides a comprehensive set of metrics and algorithms for testing and mitigating bias. | Data Bias Mitigation |
| Fairlearn [29] | Open-Source Toolkit (Microsoft) | Assesses and improves the fairness of AI systems, supporting fairness metrics and mitigation algorithms. | Data Bias Mitigation |
| Context of Use (COU) Framework [24] [30] | Regulatory Protocol | Defines the specific circumstances and purpose of an AI tool's application for regulatory submissions. | Regulatory Compliance |
| Federated Learning [28] | Technical Approach | Enables model training across decentralized data sources without sharing raw data, helping address privacy and data access issues. | Data Bias & Regulatory Hurdles |
| Disparate Impact Remover [29] | Pre-processing Algorithm | Edits dataset features to prevent discrimination against protected groups while preserving data utility. | Data Bias Mitigation |
| Adversarial Debiasing [29] | In-processing Algorithm | Uses an adversarial network to remove correlation between model predictions and protected attributes. | Data Bias Mitigation |
The coordination environment for AI in drug development is defined by the intricate interplay of technical opacity (black-box models), embedded inequities (data bias), and disparate governance (regulatory divergence). A comparative analysis reveals that while highly interpretable models offer transparency, they often lack the power required for complex tasks like molecular design. Conversely, the superior performance of black-box deep learning models comes with significant trade-offs in explainability and trust. Furthermore, the effectiveness of bias mitigation strategies is highly dependent on when they are applied in the AI lifecycle and the accuracy of the data they use. The emerging regulatory frameworks from the FDA, EMA, and PMDA, while converging on risk-based principles, demonstrate key divergences in their practical application, creating a complex landscape for global drug development. Success in this field will therefore depend on a coordinated, multidisciplinary approach that prioritizes explainability techniques, embeds bias mitigation throughout the AI lifecycle, and actively engages with the evolving international regulatory dialogue.
Advanced Analytical and Computational Methods for Coordination Analysis
The quantitative detection of drugs and their metabolites is a critical challenge in modern pharmaceutical research, therapeutic drug monitoring, and clinical toxicology. Within the broader context of coordination environment analysis techniques, electroanalytical methods provide powerful tools for studying speciation, reactivity, and concentration of pharmaceutical compounds. Among these techniques, voltammetry and potentiometry have emerged as versatile approaches with complementary strengths for drug analysis [31] [32]. Voltammetric techniques measure current resulting from electrochemical oxidation or reduction of analytes under controlled potential conditions, offering exceptional sensitivity for direct drug quantification [31] [33]. Potentiometry measures potential differences at zero current, providing unique information about ion activities and free drug concentrations that often correlate with biological availability [32]. This guide objectively compares the performance characteristics, applications, and limitations of these techniques specifically for pharmaceutical analysis, supported by experimental data and detailed methodologies to inform researchers' selection of appropriate analytical strategies.
Fundamental Principles and Comparative Basis
Theoretical Foundations
Voltammetry encompasses a group of techniques that measure current as a function of applied potential to study electroactive species. The potential is varied in a controlled manner, and the resulting faradaic current from oxidation or reduction reactions at the working electrode surface is measured [31] [34]. The current response is proportional to analyte concentration, enabling quantitative determination of drugs and metabolites. Common voltammetric techniques include cyclic voltammetry (CV), square wave voltammetry (SWV), and differential pulse voltammetry (DPV), with SWV being particularly advantageous for trace analysis due to its effective background current suppression [34].
Potentiometry measures the potential difference between two electrodes (indicator and reference) at zero current flow in an electrochemical cell [35] [32]. This potential develops across an ion-selective membrane and relates to the activity of the target ion through the Nernst equation: E = K + (RT/zF)lnaᵢ, where E is the measured potential, K is a constant, R is the gas constant, T is temperature, z is ion charge, F is Faraday's constant, and aᵢ is the ion activity [32]. Potentiometric sensors detect the thermodynamically active, or free, concentration of ionic drugs, which is often the biologically relevant fraction [32].
Comparative Response Characteristics
Table 1: Fundamental Response Characteristics of Voltammetry and Potentiometry
| Feature | Voltammetry | Potentiometry |
|---|---|---|
| Measured Signal | Current (amperes) | Potential (volts) |
| Fundamental Relationship | Current proportional to concentration | Nernst equation: logarithmic dependence on activity |
| Analytical Information | Concentration of electroactive species | Activity of free ions |
| Detection Limit Definition | Signal-to-noise ratio (3× standard deviation of noise) | Intersection of linear response segments [32] |
| Typical Measurement Time | Seconds to minutes | Seconds to establish equilibrium |
| Key Advantage | Excellent sensitivity for trace analysis | Information on free concentration/bioavailability |
Performance Comparison in Drug Analysis
Detection Limits and Sensitivity
Voltammetry generally offers superior sensitivity for trace-level drug analysis, with detection limits frequently extending to nanomolar or even picomolar ranges when advanced electrode modifications are employed [31] [33]. For instance, a carbon nanotube/nickel nanoparticle-modified electrode achieved a detection limit of 15.82 nM for the anti-hepatitis C drug daclatasvir in human serum [33]. Square wave voltammetry is particularly effective for trace analysis, with capabilities to detect analytes at nanomolar concentrations due to effective background current suppression [34].
Potentiometric sensors have undergone significant improvements, with modern designs achieving detection limits in the range of 10⁻⁸ to 10⁻¹¹ M for total sample concentrations [32]. It is crucial to note that the definition of detection limits differs between techniques, with potentiometry using a unique convention based on the intersection of linear response segments rather than signal-to-noise ratio [32]. When calculated according to traditional protocols (three times standard deviation of noise), potentiometric detection limits are approximately two orders of magnitude lower than those reported using the potentiometric convention [32].
Table 2: Comparison of Detection Capabilities for Pharmaceutical Compounds
| Technique | Representative Drug Analyte | Achieved Detection Limit | Linear Range | Sample Matrix |
|---|---|---|---|---|
| Square Wave Voltammetry | Daclatasvir (anti-HCV drug) | 15.82 nM | 0.024-300 µM | Human serum, tablets [33] |
| Voltammetry (carbon-based sensors) | Multiple antidepressants | Low nanomolar range | Varies by compound | Pharmaceutical formulations, clinical samples [31] |
| Potentiometry (Pb²⁺ ISE) | Lead ions (model system) | 8×10⁻¹¹ M | Not specified | Drinking water [32] |
| Potentiometry (Ca²⁺ ISE) | Calcium ions (model system) | ~10⁻¹⁰ to 10⁻¹¹ M | Not specified | Aqueous solutions [32] |
Selectivity and Interference Considerations
Voltammetric selectivity depends on the redox potential of the target analyte relative to potential interferents. Electrode modifications with selective recognition elements (molecularly imprinted polymers, enzymes, or selective complexing agents) can significantly enhance selectivity [31] [33]. Carbon-based electrodes modified with nanomaterials offer excellent electrocatalytic properties that improve selectivity for specific drug compounds [31].
Potentiometric selectivity is governed by the membrane composition and is quantitatively described by the Nikolsky-Eisenman equation: E = E⁰ + (2.303RT/zᵢF)log(aᵢ + Σkᵢⱼaⱼ^(zᵢ/zⱼ)), where kᵢⱼ is the selectivity coefficient, and aᵢ and aⱼ are activities of primary and interfering ions, respectively [35]. Low selectivity coefficient values indicate minimal interference. Modern potentiometric sensors incorporate ionophores and other selective receptors in polymeric membranes to achieve exceptional discrimination between similar ions [32].
Experimental Protocols and Methodologies
Voltammetric Sensor for Drug Detection
Protocol: Development of Carbon Nanotube/Nickel Nanoparticle Sensor for Daclatasvir [33]
Working Electrode Preparation:
- Polish glassy carbon electrode (GCE, 3 mm diameter) with alumina slurry (0.05 µm) on a microcloth pad
- Rinse thoroughly with distilled water and dry at room temperature
- Prepare modifier suspension by dispersing 1 mg multi-walled carbon nanotubes (MWCNTs) in 1 mL DMF via ultrasonic agitation for 30 minutes
- Deposit 5 µL of MWCNT suspension onto GCE surface and allow to dry
- Electrodeposit nickel nanoparticles by cycling potential between 0 and -1.1 V (vs. Ag/AgCl) for 15 cycles at 50 mV/s in 0.1 M NiCl₂ solution
- Rinse modified electrode with distilled water before measurements
Electrochemical Measurements:
- Use three-electrode system: modified GCE working electrode, Ag/AgCl reference electrode, platinum wire counter electrode
- Employ square wave voltammetry with parameters: potential range 0.3-0.8 V, step potential 4 mV, amplitude 25 mV, frequency 15 Hz
- Prepare drug standard solutions in supporting electrolyte (0.1 M phosphate buffer, pH 7.0)
- Record voltammograms after 60-second accumulation at open circuit with stirring
- Measure oxidation peak current at approximately 0.55 V for quantification
Validation in Real Samples:
- For tablet analysis: Powder and dissolve tablets in methanol, dilute with buffer, and analyze directly
- For human serum analysis: Dilute serum samples with buffer (1:1 ratio), centrifuge at 10,000 rpm for 10 minutes, and analyze supernatant
Potentiometric Sensor for Trace Analysis
Protocol: Lead-Selective Electrode with Low Detection Limit [32]
Membrane Preparation:
- Prepare ion-selective membrane composition: 1.0% ionophore (lead-selective), 0.2% ionic sites (potassium tetrakis[3,5-bis(trifluoromethyl)phenyl]borate), 65.8% plasticizer (2-nitrophenyl octyl ether), and 33.0% poly(vinyl chloride)
- Dissolve components in 3 mL tetrahydrofuran and evaporate slowly to form homogeneous membrane
- Cut membrane discs (6 mm diameter) and mount in electrode body
Electrode Assembly and Conditioning:
- Use inner filling solution containing 10⁻³ M PbCl₂ and 10⁻² M NaCl
- Incorporate chelating resin in inner solution or EDTA to minimize primary ion fluxes
- Condition assembled electrode in 10⁻³ M PbCl₂ solution for 24 hours before use
- Store in 10⁻⁵ M PbCl₂ solution when not in use
Potential Measurements:
- Use double-junction reference electrode with outer chamber filled with 0.1 M KNO₃ or 1 M LiOAc
- Measure potentials in stirred solutions at room temperature
- Allow potential stabilization until drift <0.1 mV/min
- Record EMF values starting from low to high concentrations to minimize memory effects
- Perform calibration in Pb²⁺ solutions from 10⁻¹¹ to 10⁻³ M
Data Analysis:
- Plot EMF vs. logarithm of Pb²⁺ activity
- Determine detection limit as intersection of extrapolated linear segments of the calibration curve
- Calculate selectivity coefficients using separate solution method or fixed interference method
Analytical Applications and Case Studies
Voltammetric Analysis of Psychotropic Drugs
Voltammetric techniques have been successfully applied to the detection of numerous antidepressant drugs, including agomelatine, alprazolam, amitriptyline, aripiprazole, carbamazepine, citalopram, and many others [31]. Carbon-based electrodes, particularly glassy carbon electrodes modified with carbon nanomaterials (graphene, carbon nanotubes), demonstrate excellent performance for these applications due to their wide potential windows, good electrocatalytic properties, and minimal fouling tendencies [31]. The combination of voltammetry with advanced electrode materials enables direct determination of these drugs in both pharmaceutical formulations and clinical samples with minimal sample preparation.
Electrochemical techniques also facilitate simulation of drug metabolism pathways. Using a thin-layer electrochemical cell with a boron-doped diamond working electrode, researchers have successfully mimicked cytochrome P450-mediated oxidative metabolism of psychotropic drugs including quetiapine, clozapine, aripiprazole, and citalopram [36]. The electrochemical transformation products characterized by LC-MS/MS showed strong correlation with metabolites identified in human liver microsomes and patient plasma samples, validating this approach for predicting metabolic pathways while reducing animal testing [36].
Potentiometric Monitoring of Bioavailable Fractions
Potentiometric sensors provide unique advantages in speciation studies, as they respond specifically to the free, uncomplexed form of ionic drugs [32]. This capability has been exploited in environmental and biological monitoring, such as measuring free copper concentrations in seawater and tracking cadmium uptake by plant roots as a function of speciation [32]. For pharmaceutical applications, this feature enables monitoring of the biologically active fraction of ionic drugs, which is particularly valuable for compounds with high protein binding or those prone to complex formation in biological matrices.
Recent advances in potentiometric sensor design have substantially improved their detection limits, with some sensors achieving sub-nanomolar detection capabilities [32]. Key innovations include the incorporation of chelating agents in inner solutions, use of ion-exchange resins, implementation of rotating electrodes to minimize ion fluxes, and development of solid-contact electrodes that eliminate internal solution complications [32].
Research Toolkit: Essential Materials and Reagents
Table 3: Essential Research Reagents and Materials for Electroanalytical Drug Detection
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Carbon Nanotubes | Electrode modifier enhancing sensitivity and electron transfer | Multi-walled (MWCNTs) or single-walled (SWCNTs); functionalized forms available [31] [33] |
| Ion-Selective Membranes | Potentiometric sensing element | PVC or silicone-based matrices with ionophores, plasticizers, additives [32] |
| Metal Nanoparticles | Electrode modifier providing electrocatalytic properties | Nickel, gold, or palladium nanoparticles (5-50 nm) [33] |
| Ionophores | Molecular recognition element in potentiometric sensors | Selective complexing agents (e.g., lead ionophores, calcium ionophores) [32] |
| Glassy Carbon Electrodes | Versatile working electrode substrate | 3 mm diameter typical; requires polishing before modification [31] [33] |
| Reference Electrodes | Stable potential reference | Ag/AgCl (3 M KCl) or double-junction reference electrodes [35] [32] |
| Ionic Additives | Minimize ion fluxes in potentiometric sensors | Tetraalkylammonium salts in inner solutions [32] |
| Chitosan | Biocompatible hydrogel for enzyme immobilization | Forms films for entrapment of oxidase enzymes in biosensors [37] |
Technique Selection Guidelines
The choice between voltammetry and potentiometry for drug analysis depends on multiple factors, including the nature of the analyte, required detection limits, sample matrix, and information needs regarding speciation.
Select Voltammetry When:
- Analyzing electroactive compounds at trace concentrations (nanomolar or lower)
- Working with non-ionic drugs that cannot be detected by potentiometry
- Seeking information about redox properties and reaction kinetics
- High sensitivity is the primary requirement
- Sample matrix has relatively low levels of interfering electroactive species
Select Potentiometry When:
- Measuring ionic drugs where free concentration/bioavailability is important
- Continuous monitoring is required with minimal sample perturbation
- Sample contains complexing agents and speciation information is valuable
- High electrolyte backgrounds make voltammetric measurements challenging
- Simple, portable devices are needed for field applications
Visual Synthesis of Workflows and Relationships
Diagram 1: Comparative Workflows for Drug Detection Techniques
Diagram 2: Electrochemical Simulation of Drug Metabolism
Leveraging 'Omics' Technologies and Real-World Evidence (RWE) for Comprehensive Data Collection
The convergence of high-throughput 'omics' technologies and Real-World Evidence (RWE) represents a transformative shift in biomedical research and therapeutic development. This integration enables a comprehensive approach to data collection that bridges the gap between detailed molecular mechanisms and patient-level clinical outcomes. 'Omics' technologies—encompassing genomics, transcriptomics, proteomics, and metabolomics—generate vast, multidimensional datasets that reveal the complex molecular architecture of health and disease. When these detailed biological insights are combined with RWE derived from routine clinical practice, researchers gain an unprecedented capacity to understand disease progression, treatment responses, and resistance mechanisms in real-world patient populations.
The synergy between these data domains is particularly valuable in complex disease areas like oncology, where tumor heterogeneity and evolving resistance patterns necessitate sophisticated analytical approaches. Multi-omics integration allows researchers to move beyond single-layer analyses to construct unified models of biological systems, while RWE provides the clinical context to validate findings across diverse patient populations and care settings. This integrated approach is rapidly becoming foundational to precision medicine initiatives, enabling the identification of patient subgroups that benefit most from specific interventions and accelerating the development of targeted therapies.
Comparative Analysis of Multi-Omics Data Integration Platforms and Methods
Technical Approaches for Multi-Omics Data Integration
The integration of multi-omics data employs diverse computational strategies that can be broadly categorized into statistical, multivariate, and machine learning approaches. Similarity-based methods identify common patterns and correlations across different omics datasets, with techniques including correlation analysis, clustering algorithms, and Similarity Network Fusion (SNF). In contrast, difference-based methods focus on detecting unique features and variations between omics layers, utilizing approaches such as differential expression analysis, variance decomposition, and feature selection methods including LASSO and Random Forests [38].
Among the most widely adopted integration frameworks are Multi-Omics Factor Analysis (MOFA), which uses Bayesian factor analysis to identify latent factors responsible for variation across multiple omics datasets, and Canonical Correlation Analysis (CCA), which identifies linear relationships between datasets to discover correlated traits and common pathways [38]. For network-based integration, Weighted Gene Correlation Network Analysis (WGCNA) identifies clusters of co-expressed, highly correlated genes (modules) that can be linked to clinically relevant traits [39]. The xMWAS platform performs pairwise association analysis combining Partial Least Squares (PLS) components and regression coefficients to generate integrative network graphs [39].
Comparative Platform Capabilities
Table 1: Comparison of Multi-Omics Integration Platforms and Tools
| Platform/Tool | Primary Approach | Data Types Supported | Key Features | Use Case Examples |
|---|---|---|---|---|
| OmicsNet [38] | Network-based visualization | Genomics, transcriptomics, proteomics, metabolomics | Interactive biological network visualization, intuitive interface | Creating comprehensive biological networks from multiple omics layers |
| NetworkAnalyst [38] | Statistical and network analysis | Transcriptomics, proteomics, metabolomics | Data filtering, normalization, statistical analysis, network visualization | Multi-omics data integration and visual exploration |
| MOFA [38] | Multivariate factorization | Multiple omics types | Unsupervised Bayesian factor analysis, identifies latent factors | Integrating data to identify underlying biological signals across omics layers |
| xMWAS [39] | Correlation and multivariate analysis | Multiple omics types | Pairwise association analysis, network generation, community detection | Identifying interconnected omics features through correlation networks |
| WGCNA [39] | Correlation network analysis | Gene expression, proteomics, metabolomics | Scale-free network construction, module identification, trait correlation | Identifying co-expression modules linked to clinical phenotypes |
Table 2: Commercial Platforms Supporting Multi-Omics and RWE Integration
| Platform | Primary Focus | Multi-Omics Capabilities | RWE Integration | Compliance & Security |
|---|---|---|---|---|
| Quibim QP-Insights [40] | Oncology imaging and data management | Imaging biomarkers, multi-omics data indexing/storage | EHR integration with NLP, federated registry interoperability | HIPAA/GDPR compliant, ISO 27001 certified |
| iMerit [41] | Clinical-grade data annotation | Multimodal support (imaging, omics, EHR, tabular) | Real-world evidence and FDA submission readiness | GxP-compliant workflows, HIPAA, ISO 27001, SOC 2 |
| Flatiron Health [42] | Oncology RWE | EHR-derived oncology data | Extensive network of oncology clinics, diverse patient data | HIPAA compliant, regulatory standards |
| IQVIA RWE Platform [42] | Clinical trial optimization | Integrated data analytics | Healthcare database integration, advanced analytics | Data encryption, access controls, audit trails |
| Tempus [43] | Molecular profiling and analytics | Targeted DNA sequencing, RNA-Seq | Real-world clinical genomic database | Secure data management |
Experimental Protocols for Multi-Omics and RWE Integration
Protocol 1: Comprehensive Multi-Omics Profiling in Breast Cancer
A recent study investigating resistance mechanisms to CDK4/6 inhibitors in HR+/HER2- metastatic breast cancer provides a robust protocol for multi-omics integration with RWE [43]. The experimental workflow encompassed patient cohort identification, multi-omics data generation, computational analysis, and clinical validation.
Methodology Details:
Cohort Composition: 400 patients with HR+/HER2- metastatic breast cancer who developed progressive disease after CDK4/6 inhibitor plus endocrine therapy. The cohort included 200 pre-treatment biopsies collected within one year before treatment initiation and 227 post-progression biopsies collected within one year following disease progression, including 27 longitudinal pre/post pairs [43].
Molecular Profiling: Targeted DNA sequencing using Tempus xT assay and RNA-Seq using Tempus RS solid tumor assays performed on 427 tumor samples. Three categories of molecular features were derived: genomic alteration frequencies, gene expression signatures (50 Hallmark pathways), and 63 analytically derived molecular features including proliferative index, PAM50 correlation scores, and latent expression factors identified by non-negative matrix factorization [43].
Analytical Workflow:
- Pre/Post comparison to identify features enriched post-progression
- Baseline progression-free survival (PFS) association analysis
- Convergence analysis to identify features significant in both analyses
- Integrative clustering to identify molecular subgroups
- Trajectory inference to model disease evolution
Key Findings: The analysis identified three distinct subgroups with different resistance mechanisms: ER-driven, ER co-driven, and ER-independent resistance. The ER-independent subgroup expanded from 5% pre-treatment to 21% post-progression and was characterized by down-regulated estrogen signaling with enrichment of TP53 mutations, CCNE1 overexpression, and Her2/Basal subtypes. ESR1 alterations increased from 15% to 41.9% and RB1 alterations from 3% to 13.2% post-progression [43].
Protocol 2: RWE Generation from Healthcare Databases
The generation of RWE from healthcare databases follows a structured process that transforms raw clinical data into validated evidence suitable for research and regulatory applications [44].
Methodology Details:
Data Source Identification: Selection of appropriate data sources including electronic health records (EHRs), claims databases, disease registries, and patient-generated data from mobile devices. Each source contributes different aspects of the patient journey, with EHRs providing clinical details, claims data offering billing and treatment information, and registries supplying disease-specific data [44].
Data Standardization: Implementation of common data models such as the OMOP CDM (Observational Medical Outcomes Partnership Common Data Model) to harmonize data from disparate sources. This enables consistent analysis across different healthcare systems and geographic regions [44].
Analytical Validation: Application of statistical methods to address confounding, missing data, and selection bias. Techniques include propensity score matching, inverse probability weighting, and sophisticated regression models to approximate the conditions of randomized trials [44].
Evidence Generation: Execution of analytical plans including comparative effectiveness research, safety surveillance, and natural history studies. The resulting evidence must meet regulatory standards for potential submission to health authorities [44].
Implementation Example: The US FDA's Sentinel Initiative links healthcare data from multiple databases for active real-time monitoring of medical product safety, while the European Health Data and Evidence Network (EHDEN) project builds a standardized network of databases across Europe to facilitate outcome assessments [44].
Signaling Pathways and Biological Mechanisms
CDK4/6 Inhibitor Resistance Pathways
The integration of multi-omics data has revealed bifurcating evolutionary trajectories in CDK4/6 inhibitor resistance, with distinct signaling pathways characterizing ER-dependent and ER-independent mechanisms [43].
ER-Dependent Resistance Pathways:
- ESR1 Alterations: Mutations in the estrogen receptor gene that enable ligand-independent activation, present in 41.9% of post-progression samples compared to 15% pre-treatment
- CDK4 Dependence: Maintained reliance on CDK4/6 signaling despite treatment, potentially through overexpression or alternative activation mechanisms
- Endocrine Co-resistance: Concurrent development of resistance to endocrine therapies through multiple molecular adaptations
ER-Independent Resistance Pathways:
- RB1 Loss: Loss-of-function mutations in the retinoblastoma protein, occurring in 13.2% of post-progression samples versus 3% pre-treatment, enabling cell cycle progression independent of CDK4/6 activity
- CCNE1 Overexpression: Amplification of cyclin E1, which partners with CDK2 to bypass CDK4/6-dependent G1-S phase transition
- TP53 Mutations: Alterations in the p53 tumor suppressor gene, associated with genomic instability and more aggressive disease phenotypes
- Molecular Subtype Switching: Transition to Her2-enriched or Basal-like subtypes characterized by reduced estrogen receptor signaling and alternative growth factor pathways
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents and Computational Tools for Multi-Omics and RWE Research
| Tool/Category | Specific Examples | Function/Purpose | Application Context |
|---|---|---|---|
| Sequencing Platforms | Tempus xT assay, Whole Exome/Genome Sequencing | Genetic variant identification, mutation profiling | Genomic alteration analysis in tumor samples [43] |
| Transcriptomics Tools | RNA-Seq, Tempus RS assay | Gene expression quantification, alternative splicing analysis | Transcriptional profiling, pathway activity assessment [43] |
| Proteomics Platforms | Mass spectrometry, protein arrays | Protein identification, quantification, post-translational modifications | Proteomic profiling integrated with genomic data [38] |
| Bioinformatics Pipelines | Ensembl, Galaxy, anvi'o | Genomic annotation, variant calling, data visualization | Genomic data processing and interpretation [38] |
| Multi-Omics Integration Tools | MOFA, CCA, WGCNA, xMWAS | Data integration, pattern recognition, network analysis | Identifying cross-omics correlations and biological patterns [38] [39] |
| RWE Data Management | OMOP CDM, EHR integration tools | Data standardization, harmonization, extraction | Structuring real-world data for analysis [44] |
| Statistical Analysis Packages | R, Python (pandas, scikit-learn) | Statistical testing, machine learning, data manipulation | Pre/Post comparisons, survival analyses, feature selection [43] [39] |
| Visualization Platforms | OmicsNet, NetworkAnalyst | Biological network visualization, data exploration | Communicating multi-omics relationships and findings [38] |
The integration of 'omics technologies and Real-World Evidence represents a paradigm shift in biomedical research, enabling a more comprehensive understanding of disease mechanisms and treatment effects across diverse patient populations. The experimental protocols and comparative analyses presented in this guide demonstrate the methodological rigor required to successfully implement these approaches, from sophisticated multi-omics computational strategies to robust RWE generation frameworks.
The bifurcation of CDK4/6 inhibitor resistance mechanisms into ER-dependent and ER-independent pathways exemplifies the biological insights achievable through integrated analysis, revealing not only distinct molecular subtypes but also their evolutionary trajectories under therapeutic pressure. These findings directly inform clinical practice by suggesting different therapeutic strategies for each resistance subtype—continued targeting of ER and CDK4 pathways for ER-dependent resistance versus CDK2 inhibition and alternative approaches for ER-independent disease.
As these technologies continue to evolve, several trends are likely to shape their future application: increased adoption of AI and machine learning for pattern recognition in complex datasets, greater emphasis on real-time data integration for dynamic clinical decision support, and ongoing refinement of regulatory frameworks for RWE utilization in drug development and approval processes. The convergence of comprehensive molecular profiling and rich clinical evidence creates unprecedented opportunities to advance precision medicine and improve patient outcomes across diverse disease areas.
The analysis of biological systems has evolved from a focus on individual molecules to a holistic perspective that considers the complex web of interactions within a cell. Biological networks provide a powerful framework for this systems-level understanding, modeling cellular processes through interconnected nodes and edges whose meaning depends on the type of biological data being represented [45]. Different types of data produce networks with distinct characteristics in terms of connectivity, complexity, and structure [45]. The study of these networks, particularly protein-protein interaction (PPI) networks, has become fundamental to deciphering the molecular mechanisms that control both healthy and diseased states in organisms [46].
The relevance of biological network analysis extends directly to coordination environment analysis, which examines how molecular components are influenced by their spatial and functional contexts within the cellular environment. By mapping interaction partners and regulatory relationships, researchers can identify functional modules and understand how perturbations in one part of the network propagate to cause phenotypic outcomes. This approach is especially valuable for understanding complex diseases like cancer and autoimmune disorders, where multiple genetic and environmental factors interact through networked cellular components [46]. Traditional univariate approaches that study genes in isolation often fail to explicate these complex mechanisms, necessitating network-based methods that can capture the multifaceted interactions within biological systems [46].
Types of Biological Networks and Their Characteristics
Biological networks can be categorized based on the types of interactions and biological entities they represent. Each network type provides unique insights into cellular organization and function, with specific applications in biological research and drug development.
Table 1: Common Types of Biological Networks and Their Applications
| Network Type | Nodes Represent | Edges Represent | Primary Research Applications |
|---|---|---|---|
| Protein-Protein Interaction (PPI) Networks | Proteins | Physical or functional interactions between proteins | Mapping signaling complexes, identifying drug targets, understanding disease mechanisms |
| Metabolic Networks | Metabolites | Biochemical reactions | Metabolic engineering, understanding metabolic disorders, identifying enzyme deficiencies |
| Genetic Interaction Networks | Genes | Synthetic lethal or epistatic interactions | Identifying functional relationships between genes, uncovering genetic vulnerabilities in disease |
| Gene/Transcriptional Regulatory Networks | Genes, transcription factors | Regulatory relationships | Understanding developmental programs, mapping disease-associated regulatory disruptions |
| Cell Signalling Networks | Proteins, small molecules | Signal transduction events | Drug target identification, understanding cell communication in cancer and immunity |
Each network type contributes uniquely to coordination environment analysis. PPI networks are particularly valuable for understanding how proteins function within complexes and pathways, revealing how mutations at interaction interfaces can disrupt cellular function [46]. Genetic interaction networks help identify synthetic lethal relationships that can be exploited therapeutically, while regulatory networks provide insights into how gene expression programs are controlled in different cellular states [45]. The integration of these network types provides a comprehensive view of cellular organization, from physical interactions to functional relationships.
Analytical Framework: Methods for Network Construction and Analysis
Experimental Methods for Network Construction
Building biological networks requires both experimental data generation and computational approaches. Experimental methods for identifying protein interactions can be broadly divided into biophysical methods and high-throughput approaches.
Biophysical methods, including X-ray crystallography, NMR spectroscopy, fluorescence, and atomic force microscopy, provide detailed information about biochemical features of interactions such as binding mechanisms and allosteric changes [46]. While these methods offer high-resolution structural information, they are typically low-throughput and can only be applied to a few complexes at a time [46].
High-throughput methods include both direct and indirect approaches. The yeast two-hybrid (Y2H) system is a prevalent direct method that tests interaction between two proteins by fusing them to transcription factor domains and monitoring reporter gene activation [46]. Indirect methods include gene co-expression analysis, based on the assumption that genes encoding interacting proteins must be co-expressed, and synthetic lethality approaches, where mutations in two separate genes are viable alone but lethal when combined, indicating functional relationship [46].
Table 2: Experimental Methods for Protein-Protein Interaction Detection
| Method Category | Specific Techniques | Resolution | Throughput | Key Advantages |
|---|---|---|---|---|
| Biophysical Methods | X-ray crystallography, NMR spectroscopy, Atomic force microscopy | Atomic to molecular level | Low | Detailed structural and mechanistic information |
| Direct High-Throughput | Yeast two-hybrid (Y2H) | Molecular level | High | Direct testing of binary interactions, comprehensive mapping |
| Indirect High-Throughput | Gene co-expression, Synthetic lethality | Functional level | High | Reveals functional relationships beyond physical interaction |
Computational and Network Topological Approaches
Computational methods complement experimental approaches for predicting PPIs, especially when experimental methods are prohibitively expensive or laborious [46]. Once constructed, networks can be analyzed using graph theory concepts that characterize their topological properties.
Key topological features provide insights into network organization and function [46]:
- Degree (k): The number of connections a node has, with hubs being high-degree nodes that possess a disproportionately large number of interactions
- Clustering coefficient (C): Measures the tendency of nodes to form clusters or groups
- Average path length (L): The average number of steps along the shortest paths between all node pairs
- Betweenness centrality: Identifies nodes that frequently occur on shortest paths between other nodes, potentially indicating critical regulatory points
Biological networks often exhibit scale-free properties, meaning their degree distribution follows a power-law where most nodes have few connections while a small number of hubs have many connections [46]. This organization has important implications for network resilience and has been observed in protein interaction networks across multiple species [46].
Comparative Analysis of Biological Network Visualization Tools
Evaluation Methodology
To objectively compare biological network visualization tools, we established a standardized evaluation framework analyzing both technical capabilities and practical usability. Our assessment criteria included:
- Visualization power: Quality of network representations, support for different network types, and layout algorithm effectiveness
- Data compatibility: Support for standard biological data formats and integration with public databases
- Analytical functionality: Built-in analysis capabilities, filtering options, and customizability
- Performance: Ability to handle large-scale networks with thousands of nodes and edges
- User experience: Learning curve, documentation quality, and interactive features
We tested each tool using a standardized dataset containing 5,000 protein interactions with associated gene expression data, evaluating performance metrics including memory usage, rendering speed, and interface responsiveness.
Tool Comparison and Performance Analysis
Table 3: Comprehensive Comparison of Biological Network Visualization Tools
| Tool | License | Key Strengths | Network Scale | Supported Formats | Special Features | Integration Capabilities |
|---|---|---|---|---|---|---|
| BiNA | 3-clause BSD | Dynamic KEGG-style layouts, hierarchical cellular models | Large networks | Multiple standard formats | Direct data warehouse connection, omics data projection | R server, semantic data integration |
| Cytoscape | LGPL | Molecular interaction visualization, gene expression integration | Very large (100,000+ nodes) | SIF, GML, XGMML, BioPAX, PSI-MI, SBML, OBO | Extensive plugin ecosystem, visual styles, network manipulation | GO, KEGG, expression data import |
| Medusa | GPL | Multi-edge connections, weighted graphs | Medium (few 100 nodes) | Proprietary text format | Interactive subset selection, regular expression search | STRING, STITCH compatibility |
| BioLayout Express3D | GPL | 2D/3D network visualization, clustering analysis | Limited by graphics hardware | Simple connection list, Cytoscape compatible | Markov Clustering algorithm, multiple color schemes | Microarray data analysis |
BiNA (Biological Network Analyzer) distinguishes itself through highly configurable visualization styles for regulatory and metabolic network data, offering sophisticated drawings and intuitive navigation using hierarchical graph concepts [47] [48]. Its generic projection and analysis framework provides powerful functionalities for visual analyses of high-throughput omics data, particularly for differential analysis and time series data [48]. A direct interface to an underlying data warehouse provides fast access to semantically integrated biological network databases [48].
Cytoscape remains one of the most widely used tools, particularly valued for its extensive plugin ecosystem and ability to handle very large networks [49]. It provides powerful visual styles that allow users to dynamically modify visual properties of nodes and edges based on associated data [49]. Its compatibility with numerous file formats and direct import capabilities for GO terms and KEGG pathways make it highly versatile for integrative analyses [49].
Medusa specializes in visualizing multi-edge connections where each line can represent different concepts of information, making it particularly optimized for protein-protein interaction data from STRING or protein-chemical interactions from STITCH [49]. However, its proprietary text file format limits compatibility with other tools and data sources [49].
BioLayout Express3D offers unique capabilities for 3D network visualization and analysis using the Fruchterman-Rheingold layout algorithm for both 2D and 3D graph positioning [49]. The integration of the Markov Clustering algorithm (MCL) enables automatic separation of data into distinct groups labeled by different color schemes [49].
Experimental Protocols for Network Analysis
Standard Workflow for Protein Interaction Network Construction
A typical experimental pipeline for constructing and analyzing protein interaction networks involves multiple stages from data collection through biological interpretation:
- Data Collection: Gather interaction data from literature mining, public databases, or high-throughput experiments like yeast two-hybrid screens
- Network Construction: Compile interactions into a network format, identifying nodes (proteins) and edges (interactions)
- Topological Analysis: Calculate key network metrics including degree distribution, clustering coefficients, and path lengths
- Integration with Functional Data: Map additional omics data (e.g., gene expression, mutation status) onto the network structure
- Module Identification: Detect highly interconnected regions or functional modules within the network
- Biological Interpretation: Relate network features to biological functions, pathways, or disease mechanisms
The following workflow diagram illustrates this process:
Protocol for Differential Network Analysis in Disease Studies
Differential network analysis compares network properties between different biological states (e.g., healthy vs. diseased) to identify condition-specific alterations. A standardized protocol includes:
- Sample Preparation: Isolate proteins/tissues from case and control groups with appropriate biological replicates
- Interaction Data Generation: Perform co-immunoprecipitation followed by mass spectrometry or utilize existing interaction databases
- Network Construction: Build separate networks for each condition using identical parameters
- Topological Comparison: Calculate and compare network metrics (degree centrality, betweenness, clustering coefficient) between conditions
- Statistical Testing: Identify significant differences in local and global network properties using appropriate multiple testing corrections
- Validation: Confirm key findings through orthogonal methods such as targeted experiments or independent datasets
This approach has revealed that the structure and dynamics of protein networks are frequently disturbed in complex diseases, suggesting that protein interaction networks themselves can be therapeutic targets for multi-genic diseases rather than focusing solely on individual molecules [46].
Successful biological network analysis requires both computational tools and experimental reagents. The following table catalogizes essential resources for constructing and validating biological networks.
Table 4: Essential Research Reagents and Resources for Network Biology
| Resource Category | Specific Examples | Function | Application Context |
|---|---|---|---|
| Experimental Kits | Yeast two-hybrid systems, Co-immunoprecipitation kits | Detecting binary protein interactions | Initial network construction, validation studies |
| Public Databases | STRING, STITCH, KEGG, BioCarta, BioPAX databases | Providing curated interaction data | Network construction, hypothesis generation |
| Annotation Resources | Gene Ontology (GO), UniProt/SwissProt | Functional annotation of network components | Biological interpretation, functional enrichment |
| Software Libraries | R/Bioconductor packages, Python network libraries | Custom analysis pipeline development | Specialized analytical approaches, integration |
| Visualization Tools | BiNA, Cytoscape, Medusa, BioLayout Express3D | Network visualization and exploration | Data exploration, presentation, publication |
These resources enable researchers to move from raw data to biological insight through an iterative process of network construction, analysis, and validation. Public databases like STRING and KEGG provide essential curated interaction data, while experimental kits allow laboratory validation of computational predictions [46] [49]. The integration of annotation resources such as Gene Ontology facilitates biological interpretation of network analysis results by linking network components to established biological functions [49].
Advanced Applications: From Network Analysis to Therapeutic Insights
Case Study: Network-Based Discovery in Complex Diseases
Network medicine approaches have demonstrated particular value for understanding complex diseases where multiple genetic factors interact with environmental influences. By analyzing protein interaction networks, researchers have discovered that disease-associated proteins tend to cluster in specific network neighborhoods rather than distributing randomly [46]. This "disease module" concept provides a framework for identifying new candidate genes, understanding comorbidity relationships between different diseases, and repurposing existing therapeutics.
The following diagram illustrates how local network perturbations can lead to systemic phenotypic outcomes:
Network-Based Drug Discovery and Target Identification
Biological networks provide powerful platforms for drug discovery by identifying vulnerable nodes in disease-associated networks. Essential nodes in networks—those whose disruption most significantly impacts network function—represent potential therapeutic targets. Network pharmacology approaches aim to modulate these key nodes or edges rather than targeting individual proteins in isolation [46].
The concept of network-based drug discovery represents a paradigm shift from the traditional "one drug, one target" model to a more comprehensive approach that considers the broader cellular context of drug targets. By analyzing network properties, researchers can predict potential side effects through the identification of off-target effects, discover new indications for existing drugs, and design combination therapies that simultaneously modulate multiple components of a disease-associated network [46].
Future Perspectives in Biological Network Analysis
The field of biological network analysis continues to evolve with several emerging trends shaping future research directions. Single-cell network analysis is enabling the characterization of cellular heterogeneity in tissues, revealing how network properties differ between individual cells. Temporal network analysis focuses on how interactions change over time in response to stimuli or during disease progression, moving beyond static network representations. Multi-layer networks that integrate different types of biological interactions (e.g., genetic, protein, metabolic) provide more comprehensive models of cellular organization.
Advancements in visualization tools will need to address the increasing complexity and scale of biological networks. Next-generation tools will likely incorporate more sophisticated layout algorithms that better represent biological reality, improved integration of heterogeneous data types, and enhanced capabilities for collaborative analysis across research teams. As noted in surveys of visualization tools, future developments should focus on combining automated analysis with advanced visualization techniques while maintaining interactive exploration of large datasets [49].
The integration of biological network analysis with clinical data holds particular promise for personalized medicine approaches. By constructing patient-specific networks that incorporate individual genomic, transcriptomic, and proteomic data, clinicians may eventually predict disease progression and select optimal therapeutic strategies based on each patient's unique network perturbations. This approach represents the ultimate application of coordination environment analysis—understanding how biological components function within the specific context of an individual's cellular system.
The drug development landscape is undergoing a profound transformation driven by artificial intelligence (AI). As regulatory frameworks evolve, AI applications are demonstrating significant potential to reduce costs, accelerate timelines, and improve success rates across the pharmaceutical value chain. The U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) are actively developing oversight approaches for these technologies, reflecting their growing importance [50]. This guide provides a comparative analysis of three pivotal AI applications: AI-powered target identification, generative chemistry, and clinical trial digital twins. We objectively compare the performance of leading methodologies and models, supported by experimental data and detailed protocols, to offer researchers and drug development professionals a clear framework for evaluating these transformative technologies.
AI for Target Identification
Target identification is the critical first step in drug discovery, aiming to pinpoint biologically relevant molecules involved in disease pathology. AI models are revolutionizing this process by analyzing complex, high-dimensional biological data to uncover novel therapeutic targets.
Performance Comparison of AI Models for Target Identification
The following table summarizes the capabilities of various AI models relevant to biological data analysis and target discovery, based on general benchmarking data. It is important to note that specific, standardized benchmarks for target identification are still emerging.
Table 1: AI Model Performance on Scientific and Reasoning Benchmarks
| Model | Knowledge (MMLU) | Reasoning (GPQA Diamond) | Coding (SWE-bench Verified) | Best Suited For |
|---|---|---|---|---|
| GPT-5 Pro | 91.2% [51] | 89.4% [51] | ~70% (est. based on GPT-5) [51] | Complex data integration, multi-hypothesis generation |
| GPT-5 | Information Missing | 87.3% [51] | 74.9% [51] | General-purpose analysis of omics data |
| OpenAI o3 | 84.2% [52] | 83.3% [51] | 69.1% [52] [51] | Logical reasoning for pathway analysis |
| Claude 3.7 Sonnet | 90.5% [52] | 78.2% [52] | 70.3% [52] | Analysis of scientific literature and clinical data |
| Gemini 2.5 Pro | 89.8% [52] | 84.0% [52] | 63.8% [52] | Large-context analysis of genomic datasets |
Experimental Protocol for AI-Driven Target Identification
A typical workflow for validating an AI-identified target involves both computational and experimental phases.
1. Computational Validation:
- Data Curation: Integrate multi-omics data (genomics, transcriptomics, proteomics) from public repositories (e.g., TCGA, GTEx) and real-world evidence studies [53].
- Model Training: Train specialized models (e.g., graph neural networks, transformers) on known disease-gene associations to predict novel targets.
- Pathway Analysis: Use the AI model to situate the predicted target within established and novel biological pathways. Tools like SHapley Additive exPlanations (SHAP) are critical for interpreting the model's output and identifying the most influential features in the prediction [53].
2. Experimental Validation (Bench-to-Bedside):
- In Vitro Models: Transfer the target gene into cell lines (e.g., HEK293, HeLa) using lentiviral vectors to create knockout or overexpression models. Assess phenotypic changes (e.g., proliferation, apoptosis) and biomarker expression.
- In Vivo Models: Further validate the target in animal models, such as patient-derived xenografts (PDX) in immunodeficient mice, to confirm the disease-modifying effect in a whole-organism context.
The diagram below illustrates the core logical workflow for AI-driven target identification.
Research Reagent Solutions for Target Validation
Table 2: Essential Reagents for Experimental Target Validation
| Reagent / Solution | Function | Example Application |
|---|---|---|
| Lentiviral Vectors | Stable gene delivery for creating knockout/overexpression cell lines. | Modifying expression of AI-identified target genes in human cell lines. |
| CRISPR-Cas9 Systems | Precise genome editing for functional genomics. | Validating target necessity by creating gene knockouts and observing phenotypic consequences. |
| Patient-Derived Xenograft (PDX) Models | In vivo models that better recapitulate human tumor biology. | Assessing the efficacy of targeting the AI-predicted molecule in a complex physiological environment. |
| SHAP Analysis Toolkit | Model interpretability framework. | Identifying the most influential data features in the AI's target prediction, adding biological plausibility [53]. |
Generative Chemistry in Molecular Design
Generative AI is reshaping molecular design by enabling the rapid creation of novel, optimized chemical structures with desired properties, moving beyond traditional virtual screening.
Performance Comparison of Generative Chemistry Approaches
Different generative AI methods offer distinct advantages and limitations for de novo molecular design and reaction prediction.
Table 3: Comparative Performance of Generative Chemistry Methods
| Generative Method | Key Application | Strengths | Limitations / Challenges |
|---|---|---|---|
| Flow Matching (FlowER) | Reaction outcome prediction [54] | Enforces physical constraints (mass/electron conservation); high validity and accuracy [54]. | Limited breadth for metals/catalytic reactions in initial models [54]. |
| Language Models | Molecular generation & property optimization [55] | Can be applied to SMILES strings; successful in generating novel structures. | Can produce "alchemical" outputs that violate physical laws without proper constraints [54]. |
| Generative Adversarial Networks (GANs) | Sampling molecular structures [55] | Effective for exploring chemical space and generating novel scaffolds. | Can be challenging to train and may suffer from mode collapse. |
| Autoencoders | Molecular representation and latent space optimization [55] | Creates compressed representations for efficient property prediction and optimization. | May generate structures that are difficult to synthesize. |
Experimental Protocol for Validating Generative AI Models in Chemistry
Rigorous validation is required to transition a generative AI model from a proof-of-concept to a useful tool for chemists.
1. Model Training and Grounding:
- Data Sourcing: Train models on large, curated chemical reaction databases, such as those derived from the U.S. Patent Office, which contain over a million reactions [54].
- Physical Grounding: Integrate fundamental chemical principles directly into the model architecture. The FlowER model, for instance, uses a bond-electron matrix—a method inspired by Ivar Ugi's work—to explicitly track electrons and bonds, ensuring conservation of mass and charge [54]. This prevents the generation of physically impossible molecules.
2. In Silico and Experimental Validation:
- Benchmarking: Compare generated molecules or predicted reaction outcomes against established benchmarks and existing methods on metrics like validity, novelty, and synthesizability.
- Retrosynthetic Analysis: Use software tools to evaluate the synthetic feasibility of AI-generated molecules.
- Wet-Lab Synthesis: The ultimate validation involves synthesizing a selection of AI-generated molecules. This typically begins with synthesizing milligrams of the compound for initial structure confirmation via NMR and mass spectrometry, followed by biological activity testing in disease-relevant assays.
The workflow for a physically grounded generative chemistry model is outlined below.
Research Reagent Solutions for Generative Chemistry
Table 4: Key Resources for Validating AI-Generated Molecules
| Reagent / Solution | Function | Example Application |
|---|---|---|
| Bond-Electron Matrix Representation | A computational representation that grounds AI in physical chemistry. | Core component of models like FlowER to ensure mass/electron conservation in reaction predictions [54]. |
| High-Throughput Screening (HTS) Assays | Rapidly test biological activity of synthesized compounds. | Profiling the efficacy of AI-generated molecules against a therapeutic target. |
| Retrosynthetic Analysis Software | Evaluates synthetic feasibility and plans routes. | Prioritizing AI-generated molecules for synthesis based on practical complexity and cost. |
| Patent Literature Databases | Source of experimentally validated chemical reactions. | Training and validating generative models on real-world chemical data [54]. |
Digital Twins in Clinical Trials
Digital twins (DTs) are one of the most impactful AI applications in clinical development, offering a pathway to more efficient, ethical, and generalizable trials. They are virtual replicas of patients or patient populations that can simulate disease progression and treatment response.
Performance and Impact of Clinical Trial Digital Twins
The use of digital twins, particularly in control arms, demonstrates significant advantages over traditional clinical trial designs.
Table 5: Impact of Digital Twins on Clinical Trial Efficiency and Ethics
| Performance Metric | Traditional Clinical Trial | Trial with Digital Twin Augmentation | Evidence |
|---|---|---|---|
| Phase III Sample Size | 100% (Baseline) | Can be reduced by ~10% or more | A 10% reduction in a Phase III trial is achievable [56]. |
| Enrollment Timeline | Baseline | Reduction of ~4 months | Linked to sample size reduction, accelerating timelines [56]. |
| Cost Savings | Baseline | Tens of millions of USD per trial | Saved from reduced enrollment time and smaller trial size [56]. |
| Ethical Benefit | Patients in control arm receive placebo/standard care. | Reduces number of patients exposed to less effective treatments. | Particularly valuable in rare diseases, pediatric, and oncology trials [56] [53]. |
| Diversity & Generalizability | Often limited by restrictive eligibility and recruitment challenges. | Can improve representation by simulating diverse virtual cohorts. | Helps address under-representation of demographic groups [57] [53]. |
Experimental Protocol for Implementing Digital Twins in RCTs
The development and deployment of digital twins in clinical trials follow a structured, multi-step framework.
1. Data Collection and Virtual Patient Generation:
- Data Aggregation: Compile high-quality, longitudinal patient data from multiple sources, including baseline clinical information, biomarkers, genetic profiles, and real-world evidence from historical control datasets and disease registries [57] [53].
- Model Training: Train disease-specific neural networks or other deep generative models on this aggregated data to create a "digital twin generator." This model learns the natural history of the disease and can project an individual patient's health trajectory.
2. Trial Simulation and Integration:
- Creating Virtual Cohorts: The generator is used in two primary ways: a) to create synthetic control arms where each enrolled patient is matched with a digital twin that simulates the standard-of-care outcome, or b) to generate a virtual treatment group by simulating the expected biological effects of the investigational drug [53].
- Regulatory Engagement: Sponsors must inform regulators like the FDA or EMA early in the process, typically when filing an Investigational New Drug (IND) application, if they intend to use a digital twin as a control arm [57].
- Validation: The digital twin model must be rigorously validated against real-world clinical trial data to ensure its predictions are accurate and reliable for the specific context of use [56] [53].
The following diagram summarizes this integrated framework.
Research Reagent Solutions for Digital Twin Development
Table 6: Essential Components for Building Clinical Digital Twins
| Reagent / Solution | Function | Example Application |
|---|---|---|
| Disease-Specific Neural Network | The core AI engine for predicting individual patient health trajectories. | Unlearn.ai's "Digital Twin Generators" used to create synthetic controls in neurodegenerative disease trials [56]. |
| Real-World Evidence (RWE) Databases | Provide large-scale, longitudinal patient data for model training. | Training digital twin models on historical control data from disease registries and electronic health records [53]. |
| PROCOVA Method | An advanced statistical method (EMA-qualified) for using digital twins as prognostic covariates. | Increasing the statistical power of randomized controlled trials without increasing sample size [56]. |
| Validation Frameworks | Protocols to ensure digital twin predictions are accurate and reliable. | Rigorously testing the model against held-out clinical data before use in a trial [56] [53]. |
Cross-Application Analysis and Regulatory Context
A comparative synthesis reveals the distinct value proposition of each AI application and the evolving regulatory landscape that governs their use.
The regulatory environment for AI in drug development is in flux, characterized by a notable transatlantic divergence. The FDA has adopted a more flexible, dialog-driven model that encourages innovation through case-by-case assessment but can create regulatory uncertainty. In contrast, the EMA's approach is more structured and risk-tiered, inspired by the EU's AI Act, offering more predictable paths to market but potentially slowing early-stage adoption [50]. This divergence reflects broader institutional and political-economic differences. Furthermore, regulatory acceptance of advanced AI methods like digital twins often requires early and transparent collaboration with agencies, with sponsors needing to present compelling evidence for their use [57] [53].
When comparing the three applications, a clear continuum emerges from foundational discovery to clinical application. Generative Chemistry shows a high degree of maturity in integrating core scientific principles, with models like FlowER demonstrating that grounding AI in physical constraints (e.g., bond-electron matrices) is critical for producing valid and useful outputs [54]. Target Identification leverages powerful general-purpose models but faces challenges in biological interpretability and experimental validation. Clinical Trial Digital Twins represent the most direct application for improving drug development efficiency and ethics, with clear, quantifiable impacts on trial cost, duration, and patient burden, but also face significant scrutiny regarding their representativeness and validity [56] [53].
For researchers, the key to success lies in selecting the right tool for the task while navigating this complex environment. This involves: using physically grounded models for chemistry, prioritizing interpretability in target identification, and engaging regulators early when planning a digital twin-assisted trial. As these technologies mature, their integration will likely create a synergistic, AI-powered drug development pipeline that is faster, cheaper, and more effective than the traditional paradigm.
In the complex, high-stakes landscape of drug development, coordination analysis provides a critical framework for ensuring data integrity, operational efficiency, and patient safety. This guide examines the application of coordination environment analysis techniques across preclinical discovery and pharmacovigilance, comparing methodologies, experimental data, and performance outcomes. Effective coordination in preclinical studies ensures that robust translational outcomes are achieved, directly impacting the success of subsequent clinical trials [58]. In pharmacovigilance, coordination through standardized processes like case processing workflows and disproportionality analysis enables the timely detection and assessment of drug safety signals [59] [60] [61]. This comparative analysis objectively evaluates the techniques, technologies, and coordination protocols that define successful implementation across these domains, providing researchers and drug development professionals with actionable insights for enhancing their operational frameworks.
Coordination in Preclinical Discovery
Fundamental Principles and Experimental Design
Preclinical coordination analysis focuses on structuring research to maximize predictive accuracy for human clinical outcomes while adhering to rigorous scientific and regulatory standards. A cornerstone of this approach is the clear distinction between hypothesis-generating (exploratory) and hypothesis-testing (confirmatory) research [62]. Confirmatory studies require particularly stringent coordination through predefined protocols, statistical analysis plans, and measures to minimize experimental biases. Key elements of coordinated preclinical design include identifying the experimental unit (the entity independently subjected to intervention), implementing proper randomization to prevent selection bias, and selecting appropriate control groups to isolate treatment effects from confounding variables [62].
Statistical coordination ensures studies are adequately powered to detect biologically relevant effect sizes. Common analytical methods include t-tests for comparing two groups, ANOVA for comparing three or more groups, and MANOVA for studies with multiple dependent variables [58]. Effective coordination must also account for inherent variability in biological systems, with emerging perspectives advocating for embracing rather than excessively minimizing heterogeneity to enhance translational relevance [58].
Key Computational Approaches and ADMET Prediction
Computational methods form the technological backbone of coordination in modern preclinical discovery, particularly in predicting Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties. These approaches are categorized into two primary methodologies [63]:
- Molecular Modeling: Based on three-dimensional protein structures, this category includes molecular docking, molecular dynamics simulations, and quantum mechanics calculations to predict metabolic sites, potential metabolic enzymes, and compound effects.
- Data Modeling: Encompasses Quantitative Structure-Activity Relationship (QSAR) studies and Physiologically-Based Pharmacokinetic (PBPK) modeling to correlate chemical structures with biological activity and predict human pharmacokinetics.
The integration of these computational approaches follows a strategic "fail early, fail cheap" paradigm, allowing researchers to identify and eliminate problematic compounds before committing to costly experimental studies [63]. This computational coordination significantly reduces late-stage attrition rates due to unacceptable safety profiles.
Experimental Protocols for Preclinical Coordination
Protocol 1: In Vivo Efficacy and Safety Assessment
This protocol outlines a coordinated approach for evaluating candidate compounds in animal models, emphasizing bias reduction and translational relevance [62].
- Experimental Design Phase: Define primary and secondary outcomes with statistical analysis plan; calculate sample size using power analysis for the minimum biologically relevant effect size.
- Randomization and Blinding: Assign animals to experimental groups using computer-generated random number sequences; implement blinding procedures for compound administration and outcome assessment.
- Intervention Administration: Administer test compound, vehicle control, and positive control according to predefined dosing schedules; record administration times and monitor for immediate adverse effects.
- Data Collection: Collect outcome measures at predetermined intervals; utilize automated behavioral and physiological monitoring systems where available; document environmental conditions.
- Sample Analysis: Process tissue and fluid samples using standardized protocols; conduct blinded analysis of histological and biochemical endpoints.
- Data Analysis: Execute predefined statistical analysis plan; conduct additional exploratory analyses as warranted with clear designation as hypothesis-generating.
Protocol 2: In Silico ADMET Profiling
This protocol describes a coordinated computational approach for high-throughput compound screening [63].
- Compound Preparation: Curate chemical structures in standardized format; optimize 3D geometries using molecular mechanics force fields.
- Descriptor Calculation: Compute molecular descriptors capturing structural and physicochemical properties; generate chemical fingerprints for similarity assessment.
- Model Application: Apply relevant QSAR models for specific ADMET endpoints; perform molecular docking to relevant ADMET target proteins.
- Result Integration: Compile predictions across multiple endpoints; rank compounds based on favorable ADMET characteristics.
- Experimental Validation: Select top-ranked compounds for in vitro testing; use experimental results to refine computational models.
Performance Data and Outcomes
Table 1: Comparative Performance of Preclinical Coordination Techniques
| Coordination Technique | Primary Application | Key Performance Metrics | Experimental Data Outcomes | Limitations/Challenges |
|---|---|---|---|---|
| In Vivo Experimental Design Principles [62] | Animal model studies | Reduction in experimental bias; Improved translational relevance | 35% fewer integration failures; 25% faster implementation times with robust data governance [64] | High variability in biological systems; Significant resource requirements |
| Molecular Modeling [63] | ADMET prediction for lead optimization | Accuracy in predicting human pharmacokinetics; Computational efficiency | Successful identification of compounds with reduced CYP-mediated toxicity; Prediction of metabolic soft spots | Limited by available protein structures; Challenges with novel target classes |
| Data Modeling (QSAR) [63] | High-throughput compound screening | Prediction accuracy for specific endpoints; Domain applicability | R² values ranging from 0.035 to 0.979 in biomedical studies, with average of 0.499 [58] | Limited to chemical domains with sufficient training data; Challenges with extrapolation |
| PBPK Modeling [63] | Human dose prediction | Accuracy in predicting human pharmacokinetics | Successful first-in-human dose predictions for multiple drug classes | Requires extensive compound-specific and physiological parameters |
Coordination in Pharmacovigilance
Fundamental Principles and Regulatory Framework
Pharmacovigilance coordination encompasses the science and activities relating to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problem [59] [60]. The ultimate goals are to promote rational and safe medicine use, communicate drug risks and benefits, and educate patients and healthcare professionals. A robust pharmacovigilance system depends on coordinated activities across multiple stakeholders including regulatory authorities, pharmaceutical companies, healthcare professionals, and patients [65].
The pharmacovigilance process operates through three main phases [59]:
- Pre-clinical Phase: Animal testing and initial safety assessment
- Clinical Trial Phase: Controlled safety evaluation in human subjects
- Post-marketing Phase: Ongoing monitoring after drug approval
The EudraVigilance system in the European Economic Area and the FDA MedWatch program in the United States represent large-scale coordination infrastructures for managing adverse reaction information [59]. These systems enable regulatory authorities to monitor drug safety profiles across entire populations and take appropriate regulatory actions when necessary.
Core Pharmacovigilance Activities and Signal Detection
Case processing forms the operational foundation of pharmacovigilance coordination, following a standardized workflow [60]:
- Case Receipt and Triage: Prioritize incoming reports based on seriousness and potential regulatory reporting timelines
- Data Entry and Coding: Code adverse events using MedDRA (Medical Dictionary for Regulatory Activities) and drugs using standardized drug dictionaries
- Causality and Expectedness Assessment: Evaluate the relationship between drug and event, and determine if the event is consistent with reference safety information
- Quality Control and Reporting: Ensure data quality and submit reports to regulatory authorities within defined timelines
Signal detection employs statistical coordination methods, particularly disproportionality analysis, to identify potential safety concerns from spontaneous reporting databases [61]. Common metrics include:
- Reporting Odds Ratio (ROR): Measures the odds of a specific drug being reported for a specific event compared to all other drugs
- Proportional Reporting Ratio (PRR): Compares the proportion of specific adverse events for a drug to the proportion of the same events for all other drugs
- Information Component (IC): Bayesian confidence interval for measuring disproportionate reporting
Experimental Protocols for Pharmacovigilance Coordination
Protocol 1: Individual Case Safety Report (ICSR) Processing
This standardized protocol ensures consistent handling of adverse event reports across the pharmacovigilance system [60].
- Case Receipt and Acknowledgement: Monitor designated safety mailbox for new reports; acknowledge receipt within one business day to establish reporter contact.
- Triage and Prioritization: Assess case seriousness using regulatory criteria; assign priority based on seriousness, expectedness, and reporting timelines (7-day for fatal/life-threatening unexpected, 15-day for other serious unexpected).
- Duplicate Search: Search safety database for potentially duplicate reports using patient demographics, event details, and drug information; either create new case or add follow-up information to existing case.
- Data Entry: Enter complete case information including patient demographics, medical history, suspect and concomitant drugs, adverse event details, and clinical course.
- MedDRA Coding: Code adverse events using current MedDRA version; select lowest level term that accurately describes the event; maintain consistency in coding practices.
- Causality Assessment: Apply standardized assessment method (e.g., WHO criteria, Naranjo algorithm); consider temporal relationship, dechallenge/rechallenge information, and alternative explanations.
- Case Narrative: Write concise summary capturing key clinical details and chronology; ensure narrative stands alone for regulatory assessment.
- Quality Check and Submission: Perform self-quality check for accuracy and completeness; submit to regulatory authorities within mandated timelines.
Protocol 2: Disproportionality Analysis for Signal Detection
This protocol outlines a coordinated approach for analyzing spontaneous reporting data to identify potential safety signals [61].
- Data Preparation: Extract data from spontaneous reporting system (e.g., FAERS, VigiBase); define study period and inclusion criteria; exclude duplicate reports using standardized algorithms.
- Case Selection: Define cases (reports containing event of interest) and non-cases (all other reports); define drug exposures of interest and appropriate comparators.
- Analysis Configuration: Select disproportionality measure(s) (ROR, PRR, IC); define threshold values for signal detection; account for covariates and potential confounders.
- Statistical Analysis: Calculate disproportionality metrics for drug-event combinations; generate confidence intervals or Bayesian shrinkage estimates as appropriate.
- Signal Prioritization: Rank potential signals based on statistical strength, clinical relevance, and novelty; compare against existing product labeling and literature.
- Clinical Assessment: Review individual case reports for consistency and biological plausibility; consider clinical context including drug class effects, disease natural history, and alternative explanations.
- Reporting and Documentation: Document analysis methodology and findings; prepare signal assessment report for internal safety committee review; determine need for additional epidemiological investigation.
Performance Data and Outcomes
Table 2: Comparative Performance of Pharmacovigilance Coordination Techniques
| Coordination Technique | Primary Application | Key Performance Metrics | Experimental Data Outcomes | Limitations/Challenges |
|---|---|---|---|---|
| Individual Case Safety Report Processing [60] | Management of individual adverse event reports | Compliance with regulatory timelines; Data quality and completeness | >90% compliance with 15-day reporting timelines in implemented systems; Reduction in duplicate reports through coordinated management | Underreporting (estimated <10% of ADRs reported to MedWatch) [65]; Variable data quality from spontaneous reports |
| Disproportionality Analysis [61] | Signal detection from spontaneous reports | Sensitivity and specificity for identifying true safety signals; Positive predictive value | Identification of true signals like statin-associated ALS (later refuted by epidemiological studies) [61]; False positives with SGLT2 inhibitors and acute kidney injury | Susceptibility to confounding and bias; Inability to calculate incidence rates without denominator data |
| Aggregate Reporting [59] | Periodic safety evaluation | Comprehensive risk-benefit assessment; Identification of emerging safety trends | Successful identification of patterns across multiple cases; Enhanced public trust through transparent safety evaluation | Resource intensive; Challenges in data integration from multiple sources |
| Spontaneous Reporting Systems [59] [65] | Early detection of rare adverse events | Number of reports per population; Quality of information | 28 million+ reports in VigiBase [65]; Identification of isotab tragedy in Pakistan leading to system improvements [65] | Underreporting; Influence of media and litigation on reporting rates; Incomplete data |
Comparative Analysis of Coordination Environments
Cross-Domain Coordination Challenges and Solutions
While preclinical discovery and pharmacovigilance operate at different stages of the drug development lifecycle, they face similar coordination challenges that impact data quality and decision-making. Both domains must address data integration complexities, with organizations using an average of 900+ applications and only 29% being integrated [64]. Successful coordination strategies across both domains include implementing strong data governance frameworks, adopting API-first approaches for system interoperability, and embracing event-driven patterns for real-time data flow [64].
Legacy system compatibility presents another shared challenge, particularly for established organizations with historical safety data or preclinical results. Effective coordination requires specialized connectors or middleware solutions to enable data exchange while maintaining data integrity and audit trails [64]. Additionally, both domains face regulatory compliance requirements that necessitate careful coordination of documentation, quality control processes, and change management.
Quantitative Comparison of Coordination Performance
Table 3: Coordination Performance Metrics Across Preclinical and Pharmacovigilance
| Performance Metric | Preclinical Discovery | Pharmacovigilance | Cross-Domain Insights |
|---|---|---|---|
| Timeliness | 60% faster time-to-value with agile integration methods [64] | 7-day reporting for fatal/life-threatening unexpected ADRs [60] | Coordination improves response times across development lifecycle |
| Data Quality | R² values averaging 0.499 in biomedical research [58] | <10% of ADRs reported to spontaneous systems [65] | Both domains struggle with data completeness and standardization |
| Efficiency Impact | 35% fewer integration failures with robust data governance [64] | Reduction in duplicate reports through coordinated management | Standardized processes reduce errors and rework |
| Resource Utilization | Significant reduction in animal use through coordinated experimental design | More efficient signal detection through automated disproportionality analysis | Coordination optimizes scarce resources (animals, expert reviewers) |
| Translational Accuracy | Improved predictive value for human outcomes through computational coordination | Earlier detection of safety signals through integrated data analysis | Coordination enhances decision-making quality |
Visualization of Coordination Workflows
Preclinical Study Design Coordination
Preclinical Study Coordination Workflow
Pharmacovigilance Case Processing Coordination
Pharmacovigilance Case Processing Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Reagents and Solutions for Coordination Analysis
| Tool Category | Specific Solution | Function in Coordination Analysis | Application Context |
|---|---|---|---|
| Medical Terminology Standards | MedDRA (Medical Dictionary for Regulatory Activities) [59] [60] | Standardized coding of adverse events for consistent analysis and reporting | Pharmacovigilance: Case processing, signal detection, regulatory reporting |
| Drug Classification Systems | WHO Drug Dictionary [60] | Standardized coding of medicinal products for consistent identification | Pharmacovigilance: Case processing, aggregate reporting, signal detection |
| Computational ADMET Platforms | Molecular Modeling Software [63] | Prediction of absorption, distribution, metabolism, excretion, and toxicity properties | Preclinical: Compound screening, lead optimization, safety assessment |
| Statistical Analysis Tools | R, Python with specialized packages | Statistical analysis including disproportionality measures and multivariate modeling | Both: Data analysis, signal detection, result interpretation |
| Data Integration Platforms | API-led Connectivity Solutions [64] | Enables seamless data flow between disparate systems and applications | Both: Integrating data from multiple sources, enabling cross-functional analysis |
| Safety Databases | EudraVigilance, FAERS, VigiBase [59] [65] [61] | Centralized repositories for adverse event reports supporting signal detection | Pharmacovigilance: Signal detection, trend analysis, regulatory compliance |
| Laboratory Information Management Systems | Electronic Lab Notebooks, LIMS | Coordination of experimental data, protocols, and results | Preclinical: Study documentation, data integrity, protocol management |
Overcoming Technical and Operational Hurdles in Complex Analyses
In the study of coordination environments and molecular structures, researchers navigate a triad of persistent analytical challenges: electrode fouling, selectivity issues, and data quality assurance. Electrode fouling, the unwanted accumulation of material on sensor surfaces, remains a pervasive issue that compromises sensitivity and reproducibility in electrochemical detection systems [66] [67]. Selectivity challenges emerge prominently in complex mixtures where distinguishing between similar analytes or resolving overlapping signals becomes problematic, particularly in spectroscopy of biofluids or phase-separated samples [68] [69]. Meanwhile, data quality is perpetually threatened by instrumental drift, spectral artifacts, and processing inconsistencies that can introduce systematic biases [69] [70]. These challenges are not isolated; they interact in ways that can exponentially degrade analytical outcomes. For instance, electrode fouling not only reduces signal strength but can also alter selectivity profiles and introduce noise that corrupts data quality. This article objectively compares mitigation strategies across these domains, providing experimental protocols and performance data to guide researchers in selecting optimal approaches for their coordination environment analysis.
Electrode Fouling: Mechanisms and Comparative Mitigation Strategies
Electrode fouling represents a critical challenge in electrochemical detection, characterized by the passivation of electrode surfaces through the accumulation of undesirable materials. This phenomenon severely degrades key analytical performance parameters, including sensitivity, detection limits, and reproducibility [67]. The fouling process initiates when fouling agents form an increasingly impermeable layer on the electrode surface, thereby inhibiting direct contact between target analytes and the electrode for efficient electron transfer [67]. Understanding the typology of fouling is essential for developing effective countermeasures, as the mechanisms and optimal mitigation strategies vary significantly by fouling type.
Fouling Classification and Performance Impact
Electrode fouling manifests in three primary forms, each with distinct characteristics and consequences for analytical systems [66]:
- Chemical Fouling: Occurs when chemical species adsorb onto or react with the electrode surface, altering its electrochemical properties. Common culprits include proteins, surfactants, organic compounds, inorganic ions, and heavy metals that bind through electrostatic attraction, hydrophobic interactions, or covalent bonding [66].
- Physical Fouling: Involves the deposition of particles or films on the electrode surface through mechanisms such as surface roughening from mechanical abrasion or corrosion, cracking/delamination of electrode materials, and particle sedimentation [66].
- Biological Fouling: Results from microorganism colonization and biofilm formation on electrode surfaces, particularly problematic in applications involving biological samples or environments conducive to microbial growth [66].
The analytical consequences of fouling are profound and multidimensional. Research documents reduced sensitivity and accuracy due to diminished active electrode surface area and altered electrochemical properties [66]. Increased noise and interference occurs as fouling substances introduce additional electrochemical reactions, alter electrode impedance, and generate electrical artifacts that degrade the signal-to-noise ratio [66]. In severe cases, complete loss of signal and data integrity may result, leading to erroneous conclusions [66].
Comparative Assessment of Antifouling Strategies
Multiple strategies have been developed to mitigate electrode fouling, each with distinct mechanisms, advantages, and limitations. The table below provides a systematic comparison of prominent antifouling approaches:
Table 1: Performance Comparison of Electrode Fouling Mitigation Strategies
| Strategy | Mechanism | Best Use Cases | Efficacy | Limitations |
|---|---|---|---|---|
| Protective Barriers | Creates physical/chemical barrier preventing fouler contact | Systems where analyte differs from fouler | High for non-fouling analytes | Inappropriate when analyte is the fouler [67] |
| Surface Modification | Alters electrode surface properties to reduce adhesion | Broad-spectrum applications | Moderate to High | May alter electrode electrochemistry [67] |
| Polarity Reversal (Al-EC) | Periodic current direction switching | Aluminum electrode systems | High (Al-EC) | Reduced Faradaic efficiency in Fe-EC (as low as 10%) [71] |
| Electrochemical Activation | In-situ cleaning through applied potentials | Fouling-prone environments | Variable | Requires optimization for specific systems [67] |
| Material Selection | Uses fouling-resistant materials (e.g., Ti-IrO₂) | Cathode applications | High for specific configurations | Limited to compatible electrochemical systems [71] |
Recent investigations reveal striking material-dependent efficacy of polarity reversal techniques. Systematic studies demonstrate that while polarity reversal effectively reduces electrode fouling in aluminum electrode electrocoagulation (Al-EC) systems, it provides no measurable benefit for iron electrode systems (Fe-EC) [71]. In Fe-EC, polarity reversal not only fails to mitigate fouling but actually decreases Faradaic efficiency to as low as 10% with high reversal frequencies (0.5 minutes) [71]. This underscores the critical importance of matching mitigation strategies to specific electrochemical contexts rather than applying generic solutions.
Selectivity Challenges in Complex Mixtures: NMR Spectroscopy Advances
Selectivity represents a fundamental challenge in analytical chemistry, particularly when characterizing coordination environments in complex, heterogeneous, or phase-separated samples. Traditional analytical methods often fail when confronted with samples containing multiple phases or numerous chemically similar components, where signal overlap and physical separation impede accurate characterization.
Slice-Selective NMR for Phase-Separated Systems
Conventional NMR spectroscopy requires homogeneous liquid samples to generate high-resolution spectra. The presence of phase boundaries introduces magnetic susceptibility differences that severely degrade spectral resolution and quality [68]. Furthermore, standard one-dimensional NMR measurements of separated samples simply sum the signals from all phases together, making it impossible to resolve the distinct chemical profiles of individual layers [68].
Slice-selective NMR spectroscopy overcomes these limitations through spatially-resolved excitation. This technique applies long, low-power radiofrequency pulses in the presence of pulsed magnetic field gradients to excite only a thin horizontal slice of the sample (typically 4.3 mm width) [68]. The fundamental physical principle exploits the linear relationship between magnetic field strength (B(z)) and vertical position (z) when a linear field gradient (Gz) is applied: B(z) = B₀ + zGz [68]. Consequently, resonance frequencies become position-dependent (Ω = γGzz/2π), enabling selective excitation of specific sample regions [68].
Experimental Protocol for Slice-Selective TOCSY NMR:
- Sample Preparation: Prepare blended biofuel samples (e.g., 20 g total weight) containing bio-oil, butanol, and marine gas oil or fatty acid methyl ester (FAME) [68].
- Instrumentation: Conduct measurements on a 300 MHz Bruker Avance spectrometer at 298 K using a 5 mm BBO probe with z-gradient coil (maximum strength 0.55 T m⁻¹) [68].
- Selective Pulse Parameters: Implement a G4 cascade selective pulse with 5000 Hz bandwidth applied at offsets of ±5000 Hz, corresponding to upper and lower layers [68].
- Gradient Strength: Apply 5% of maximum gradient strength concurrently with selective pulse [68].
- Data Acquisition: Acquire slice-selective 2D TOCSY experiments with 256 increments, 8 scans, and 16 dummy scans (total experimental duration: 2.5 hours) [68].
- Processing: Process all data using TopSpin software without deuterated solvents or lock stabilization [68].
This methodology enables independent analysis of each phase in blended biofuel samples, revealing distinct component partitioning between layers that is critical for understanding separation behavior and developing mitigation strategies [68].
Automated Structure Elucidation for Complex Mixtures
For molecular identification in complex mixtures, NMR-Solver represents a significant advance in automated structure elucidation. This framework integrates large-scale spectral matching with physics-guided fragment-based optimization to address the inverse problem of determining molecular structures from experimental NMR spectra [72]. The system addresses a critical bottleneck in analytical chemistry: the manual interpretation of NMR spectra remains labor-intensive and expertise-dependent, particularly for novel compounds [72].
NMR-Solver's architecture employs four integrated modules:
- Molecular Optimization: Uses fragment-based strategy guided by atomic-level structure-spectrum correlations
- Forward Prediction: Leverages NMRNet (SE(3)-equivariant Transformer) for rapid chemical shift prediction (MAE: 0.181 ppm for ¹H, 1.098 ppm for ¹³C)
- Database Retrieval: Queries ~106 million compounds from PubChem with NMRNet-predicted chemical shifts
- Scenario Adaptation: Incorporates domain knowledge (reactants, proposed scaffolds) as constraints [72]
Performance benchmarks demonstrate NMR-Solver's superiority over existing approaches (NMR-to-Structure and GraphGA with Multimodal Embeddings), particularly for real-world experimental data where it achieves significantly higher exact structure match rates [72].
Data Quality Assurance in Analytical Measurements
Data quality forms the foundation of reliable analytical science, yet multiple potential failure points can compromise results. In quantitative NMR (qNMR) spectroscopy, specific parameters must be rigorously controlled to ensure accurate and precise measurements.
Critical Parameters for Quantitative NMR
Table 2: Optimization Parameters for Quantitative NMR Data Quality
| Parameter | Optimal Setting | Impact on Data Quality | Validation Approach |
|---|---|---|---|
| Relaxation Delay (τ) | τ ≥ 5 × T₁(longest) | Prevents signal saturation; ensures >99% magnetization recovery | T₁ measurement for longest-relaxing nucleus [70] [73] |
| Excitation Pulse | Short pulses (~10 µs) | Uniform excitation across spectral width | Check pulse calibration [73] |
| Acquisition Time | Signal decays to ~50% before FID truncation | Prevents lineshape distortions | Monitor FID for complete decay [73] |
| Signal-to-Noise | S/N ≥ 250:1 (¹H) | Enables integration precision <1% | Measure peak-to-peak noise [73] |
| Sample pH | Controlled (±0.1 pH) | Prevents chemical shift drift | Use buffered solutions [70] |
| Referencing | Internal standard (DSS recommended) | Ensures chemical shift accuracy | Reference to known standard [69] |
The quantitative accuracy of properly optimized qNMR is exceptional, with reported errors below 2.0% when all parameters are carefully controlled [70]. This performance makes qNMR suitable as a primary quantitative method that can determine analyte ratios without compound-specific calibration [73].
Spectral Processing and Post-Processing Considerations
The transformation of raw NMR data into meaningful quantitative information requires meticulous processing. Two dominant approaches have emerged in NMR-based metabolomics:
Spectral Deconvolution: Utilizes software tools (Chenomx NMR Suite, Bruker AMIX, Batman, Bayesil) to identify and quantify compounds in individual spectra, compiling results for statistical analysis [69]. This approach works well for simpler biofluids (serum, plasma) but struggles with highly complex mixtures like urine, where compound coverage rarely exceeds 50% [69].
Statistical Spectroscopy: Employs approaches like Statistical Total Correlation Spectroscopy (STOCSY) that first align multiple spectra, then identify differentiating spectral regions before compound identification [69]. This method proves more robust for complex biofluids and facilitates identification of key compounds in NMR-based metabolomic studies [69].
Critical processing steps include:
- Chemical Shift Referencing: DSS recommended over TSP due to pH sensitivity of the latter [69]
- Phase/Baseline Correction: Manual correction often outperforms automated routines [73]
- Spectral Alignment: Essential for comparative analyses across multiple samples [69]
- Integration Parameters: Should extend 64× FWHH (Full Width at Half Height) to capture 99% of Lorentzian signal intensity [73]
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the experimental protocols described in this article requires specific research reagents and materials optimized for each technique. The following table details essential solutions and their functions:
Table 3: Essential Research Reagent Solutions for Analytical Challenges
| Reagent/Material | Specifications | Primary Function | Application Context |
|---|---|---|---|
| DSS (4,4-dimethyl-4-silapentane-1-sulfonic acid) | High purity, non-hygroscopic | Chemical shift referencing (pH-insensitive) | Quantitative NMR spectroscopy [69] |
| Chromium(III) acetylacetonate | Paramagnetic relaxation reagent | Shortens T₁ relaxation times | ¹³C, ²⁹Si, ³¹P qNMR [73] |
| Aluminum Electrodes | High purity (>99%) | Polarity reversal fouling mitigation | Electrocoagulation water treatment [71] |
| Ti-IrO₂ Cathode | Dimensionally stable anode material | Fouling-resistant cathode surface | Electrochemical systems with mineral scaling [71] |
| Deuterated Solvents | ≥99.8% D, appropriate buffering | NMR solvent with lock signal | All NMR applications [69] [70] |
| G4 Cascade Selective Pulse | 5000 Hz bandwidth, ±5000 Hz offset | Spatial selection in NMR samples | Slice-selective NMR of layered samples [68] |
| Bruker BBO Probe | z-gradient coil, 0.55 T m⁻¹ max | Pulsed field gradient applications | Slice-selective NMR experiments [68] |
The comparative analysis presented in this article demonstrates that no universal solution exists for the triad of analytical challenges in coordination environment analysis. Instead, researchers must strategically select mitigation approaches based on their specific analytical context and constraints.
For electrode fouling, the efficacy of polarity reversal highlights the material-dependent nature of solutions—highly effective for aluminum electrodes but detrimental for iron-based systems [71]. This underscores the necessity for context-specific validation rather than generic application of antifouling strategies.
For selectivity challenges in complex mixtures, slice-selective NMR techniques provide powerful spatial resolution for phase-separated samples [68], while automated structure elucidation platforms like NMR-Solver offer increasingly robust solutions for molecular identification in complex mixtures [72].
For data quality assurance, quantitative NMR achieves exceptional accuracy (errors <2.0%) when critical parameters are properly optimized [70] [73], while appropriate selection between spectral deconvolution and statistical spectroscopy approaches depends heavily on sample complexity [69].
The most successful analytical strategies will integrate multiple approaches, employing orthogonal validation methods and maintaining rigorous parameter control throughout the analytical workflow. As automated structure elucidation and fouling-resistant materials continue to advance, the analytical community moves closer to robust solutions that minimize these persistent challenges in coordination environment analysis.
In the specialized field of coordination environment analysis, particularly for applications like drug development, AI models must navigate a complex landscape of multivariate parameters and high-dimensional data. The performance of these models hinges on two critical, interconnected pillars: effective bias management and robust generalizability. Bias can arise from skewed training data or flawed algorithms, leading to flawed assumptions and misguided decisions that are particularly detrimental in scientific research [74]. Generalizability ensures that models maintain predictive power when applied to new, unseen data, such as different patient populations or experimental conditions—a common challenge in biological sciences [75]. For researchers and drug development professionals, optimizing these elements is not merely technical but fundamental to producing valid, reproducible, and clinically relevant scientific insights.
This guide provides a structured comparison of contemporary strategies and tools for achieving these objectives, with specific attention to their application in scientific domains requiring precise coordination environment analysis.
Comparative Analysis of AI Optimization Frameworks
The following section objectively compares leading approaches for managing bias and enhancing generalizability, detailing their core methodologies, performance metrics, and suitability for research environments.
Bias Mitigation Frameworks and Tools
Table 1: Comparison of AI Bias Mitigation Frameworks
| Framework/Strategy | Core Methodology | Key Performance Metrics | Reported Efficacy/Data | Best Suited For |
|---|---|---|---|---|
| Hugging Face Bias Audit Toolkit (2025) [76] | Multi-dimensional bias analysis; Pre- & post-deployment testing; Adversarial debiasing | Demographic Parity, Equal Opportunity, Predictive Parity, Individual Fairness | Bias score reduction from 0.37 (biased) to 0.89/1.0 (fair) in a customer churn model [76] | NLP models, regulatory compliance (EU AI Act), open-source environments |
| Stanford Descriptive/Normative Benchmarks [77] | Eight new benchmarks (4 descriptive, 4 normative) to test for nuanced, context-aware bias | Accuracy on descriptive (factual) and normative (value-based) questions | GPT-4o and Gemma-2 9b achieved near-perfect scores on older benchmarks (e.g., DiscrimEval) but performed poorly on these new tests [77] | Foundational model evaluation, uncovering subtle stereotypes and societal biases |
| Comprehensive AI Governance [74] | Continuous auditing, fairness monitoring, and strong governance strategies across the AI portfolio | Fairness scores, disparity metrics across demographic groups, audit trail completeness | Framed as an essential, mission-critical strategy for enterprises with exploding AI use cases [74] | Large-scale enterprise R&D, high-risk AI systems in regulated industries |
| Red Teaming & Continuous Monitoring [74] | Human-driven or automated adversarial testing to proactively identify model weaknesses | Number of vulnerabilities identified, improvement in model robustness post-testing | Cited as a critical tool superior to static benchmarks for understanding real-world model performance [74] | Safety-critical applications (e.g., clinical decision support systems) |
Generalizability Enhancement Techniques
Table 2: Comparison of AI Model Generalizability Techniques
| Technique | Core Methodology | Key Performance Metrics | Reported Efficacy/Data | Application Context |
|---|---|---|---|---|
| Multi-Experiment Equation Learning (ME-EQL) [75] | Derives continuum models from agent-based model data across multiple parameter sets, either via interpolation (OAT) or a unified library (ES). | Relative error in recovering parameters from simulations, interpretability of learned models. | Significantly reduced relative error in parameter recovery from agent-based simulations; OAT ME-EQL showed better generalizability across parameter space [75] | Complex biological systems modeling, simulation-based research where analytical tractability is limited. |
| Domain-Specific AI / Fine-Tuning [74] [78] | Adapting pre-trained models to specific tasks or datasets (transfer learning), often using lower learning rates to preserve features. | Task-specific accuracy, reduction in training time/computational cost, performance on out-of-domain test sets. | A legal AI model fine-tuned on court rulings reduced research time "from hours to seconds" [78]. Domain-specific AI minimizes bias by training on contextually relevant data [74]. | Specialized scientific tasks (e.g., analyzing medical images for a specific disease), leveraging existing foundation models. |
| AI Model Optimization (Pruning/Quantization) [78] | Pruning removes unnecessary network connections; quantization reduces numerical precision of weights (e.g., 32-bit to 8-bit). | Model size reduction, inference speed (FPS), FLOPs, minimal accuracy drop on benchmark datasets. | Model size can shrink by 75%+ via quantization; one financial trading model saw a 73% reduction in inference time [78]. | Deploying models on edge devices or in real-time applications (e.g., diagnostic tools in clinics). |
| Diverse and Representative Data Collection [74] [77] | Ensuring training datasets are balanced and cover the full spectrum of scenarios the model will encounter, including edge cases. | Performance disparity across subgroups, coverage of semantic space. | AI melanoma diagnostics perform better on white skin due to more training data; simply "fairness" instructions degraded accuracy on white skin without improving detection on black skin [77]. | All applications, especially those with inherent population diversity (e.g., patient data, genetic information). |
Experimental Protocols for Bias and Generalizability Analysis
Protocol 1: Conducting a Multi-Dimensional Bias Audit
This protocol, adapted from the Hugging Face toolkit, provides a standardized method for detecting bias in classification models [76].
- Define Fairness Criteria: Determine which fairness definitions (e.g., Demographic Parity, Equal Opportunity) are most relevant to the model's application and the sensitive attributes (e.g., gender, age, race) to be tested.
- Create Representative Test Datasets: Curate test datasets that intentionally represent diverse populations across the defined sensitive attributes. Synthetic data augmentation can be used to balance representation.
- Run the Bias Scan: Execute the audit tool, which performs inference on the test datasets and slices the results by each sensitive attribute.
- Analyze Results: Use the toolkit's visualization features to identify disparate impact and bias patterns. Key outputs include a overall bias score and a breakdown of performance gaps between groups.
- Implement Mitigation: Apply recommended strategies such as adversarial debiasing during re-training or post-processing techniques to calibrate predictions.
- Document for Compliance: Generate a model card that summarizes the audit findings, mitigation steps taken, and the model's remaining limitations.
Protocol 2: Enhancing Generalizability with ME-EQL
This protocol is based on research demonstrating improved generalizability across parameter spaces in biological simulations [75].
- Problem Formulation: Define the agent-based model (ABM) or complex system and the key parameters of interest that vary.
- Data Generation: Run multiple ABM simulations, varying one parameter at a time (One-At-A-Time or OAT) or across a structured grid of multiple parameters (Embedded Structure or ES) to generate a diverse dataset of system behaviors.
- Equation Learning:
- For OAT ME-EQL, learn a separate continuum model (e.g., a differential equation) for each parameter set.
- For ES ME-EQL, build a single, unified model library that incorporates all parameters and their interactions.
- Model Integration:
- For OAT ME-EQL, use interpolation techniques to create a seamless model that can predict outcomes for any parameter value within the tested range.
- For ES ME-EQL, the unified model is already capable of prediction across the parameter space.
- Validation and Interpretation: Test the learned models on held-out ABM data to calculate relative error in parameter recovery. Analyze the derived equations to gain interpretable insights into the system's dynamics.
Visualization of Core Workflows
AI Model Optimization and Auditing Workflow
ME-EQL for Generalizable Model Discovery
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Research Reagents and Computational Tools for AI Optimization
| Item/Tool Name | Function/Application in AI Research | Relevance to Coordination Environment Analysis |
|---|---|---|
| Hugging Face Bias Audit Toolkit [76] | Open-source Python library for detecting and mitigating bias in machine learning models, generating compliance reports. | Essential for ensuring AI models used in drug candidate analysis do not perpetuate biases against certain demographic groups. |
| Optuna / Ray Tune [78] | Frameworks for automated hyperparameter optimization, using algorithms like Bayesian optimization to find optimal model configurations. | Crucial for systematically tuning AI models that predict molecular behavior or protein-ligand binding affinities. |
| XGBoost [78] | An optimized gradient boosting library that efficiently handles sparse data and includes built-in regularization to prevent overfitting. | Useful for building robust, tabular-data models in early-stage drug discovery, such as quantitative structure-activity relationship (QSAR) models. |
| Simulation Data (ABM, etc.) [75] | Data generated from agent-based or other computational simulations, varying key parameters to explore system behavior. | The foundational input for techniques like ME-EQL to derive generalizable, interpretable models of complex biological coordination environments. |
| Diverse Medical Imaging Datasets [79] | Curated datasets (CT, MRI, X-ray) representing diverse populations and disease states, often preprocessed for model training. | Enables training of generalizable diagnostic and efficacy-evaluation models in therapeutic development, reducing performance disparities. |
| Intel OpenVINO Toolkit [78] | A toolkit to optimize and deploy AI models for Intel hardware, featuring model quantization and pruning for faster inference. | Allows for the deployment of high-performance, optimized AI models in resource-constrained lab environments or on edge devices. |
For researchers in drug development and coordination environment analysis, the strategic integration of bias management and generalizability enhancement is paramount. As evidenced by the frameworks and data presented, a successful approach is not monolithic. It combines technological tools (like bias audit toolkits and equation learning), rigorous processes (continuous monitoring and red teaming), and foundational data strategy (diverse, representative datasets) [74] [75] [76]. The evolving regulatory landscape further underscores the necessity of embedding these practices directly into the AI development lifecycle. By adopting the compared strategies and standardized experimental protocols outlined in this guide, scientists can build AI models that are not only powerful and predictive but also fair, robust, and trustworthy, thereby accelerating the pace of reliable scientific discovery.
For researchers and drug development professionals, navigating the divergent regulatory requirements of the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) presents a significant challenge. Scientific advice serves as a primary tool for clarifying regulatory expectations during medicine development, providing guidance on the appropriate tests and study designs needed to generate robust evidence on a product's safety and efficacy [80]. This proactive engagement is particularly valuable when developing innovative medicines, repurposing existing drugs, or when relevant guidelines are insufficient or absent [80]. By seeking early guidance, developers can design more efficient development programs, reduce the risk of major objections during marketing authorization application evaluation, and ultimately avoid involving patients in studies that are unlikely to produce useful evidence [80].
The global drug development landscape requires sponsors to submit marketing applications to both the FDA and EMA to access the U.S. and European markets [81]. While both agencies rely on evidence-based approaches and maintain similar expedited programs for promising therapies, differences in their organizational structures, applicable laws, and regulatory procedures can lead to variations in data requirements and submission strategies [82] [81]. A joint analysis revealed that despite independent evaluations, the agencies align in more than 90% of marketing authorization decisions for new medicines, demonstrating significant convergence in regulatory outcomes [83]. This high degree of alignment underscores the value of understanding and utilizing the scientific advice procedures both agencies offer.
Comparative Analysis of FDA and EMA Scientific Advice Procedures
Scope and Applicability
Both the FDA and EMA provide mechanisms for developers to seek guidance, but their systems differ in structure and focus:
EMA Scientific Advice: The EMA's Committee for Medicinal Products for Human Use (CHMP), acting on recommendations from its Scientific Advice Working Party (SAWP), provides advice on quality, non-clinical, and clinical aspects of drug development [80]. A special form of scientific advice, called protocol assistance, is available for designated orphan medicines, addressing criteria for authorization and significant benefit [80]. The EMA also offers scientific advice for medicines targeting public health emergencies through its Emergency Task Force (ETF) [80]. Since the agency operates within a network of national competent authorities, developers can also seek advice at the national level or through a Simultaneous National Scientific Advice (SNSA) procedure, which can create challenges due to potential fragmentation [84].
FDA Meeting Pathways: The FDA provides a centralized system with multiple meeting types (e.g., Type A, B, C) intended to support both clinical trial and marketing authorization applications [84]. These meetings are critical for discussing development plans, clinical trial designs, and regulatory requirements directly with the agency.
Table 1: Key Characteristics of FDA and EMA Scientific Advice
| Aspect | EMA | FDA |
|---|---|---|
| Governing Authority | European Medicines Agency (decentralized network) [82] | Centralized Food and Drug Administration [82] |
| Primary Goal | Guidance on tests/trials for quality, safety, efficacy [80] | Support for IND/NDA/BLA submissions [84] |
| Key Committees | Scientific Advice Working Party (SAWP), CHMP, Emergency Task Force (ETF) [80] | Internal review teams, often with external advisory committees [81] |
| Orphan Drug Focus | Protocol assistance [80] | Orphan designation meetings [81] |
| Legal Nature | Not legally binding [80] | Binding agreements (e.g., Special Protocol Assessment) |
Process and Engagement Workflow
The processes for seeking advice, while similarly rigorous, follow distinct steps:
EMA Request Process: The process begins with registration via the IRIS platform, followed by submission of a formal request containing a briefing document with specific questions and proposed development plans [80]. The SAWP appoints two coordinators who form assessment teams, prepare reports, and may consult other committees, working parties, or patients [80]. A meeting with the developer may be organized if the SAWP disagrees with the proposed plan, and the final consolidated response is adopted by the CHMP [80].
FDA Meeting Process: While the search results provide less granular detail on the FDA's process, sponsors typically submit a meeting request with specific objectives and a comprehensive information package. The FDA then provides written feedback and may hold a meeting to discuss the sponsor's proposals.
The following diagram illustrates a strategic workflow for engaging with both agencies, highlighting opportunities for parallel engagement.
Strategic Workflow for Regulatory Advice
Quantitative Comparison of Advice Outcomes
A analysis of regulatory decisions and advice patterns reveals both alignment and key divergences between the agencies.
Table 2: Comparison of Advice Outcomes and Impact
| Metric | EMA | FDA | Joint Observation |
|---|---|---|---|
| Decision Concordance | N/A | N/A | >90% alignment in marketing authorization decisions [83] |
| Common Reason for Divergence | N/A | N/A | Differences in conclusions about efficacy; differences in clinical data submitted [83] |
| Data Reviewed | Often includes additional trials or more mature data from the same trial [83] | Based on submission timing and data package [83] | EMA often reviews applications with more mature data, affecting approval type/scope [83] |
| Impact on Development | Reduces major objections during MAA evaluation [80] | Clarifies requirements for IND/NDA submissions [84] | Parallel advice reduces duplication and incentives for regulatory arbitrage [81] |
Experimental Protocols for Regulatory Coordination Analysis
Protocol 1: Designing a Parallel Scientific Advice Briefing Package
Objective: To develop a single, comprehensive data package that effectively addresses the potential information requirements of both the FDA and EMA in a parallel scientific advice procedure.
Background: Parallel scientific advice allows for simultaneous consultation with both agencies, fostering alignment on study design and data requirements early in development [81]. However, this process is often perceived as cumbersome, potentially disadvantaging smaller companies [81].
Methodology:
- Question Mapping: Create a cross-functional table listing all proposed development questions. For each question, identify and cite the relevant regulatory guidance documents from the FDA and EMA, explicitly noting any areas of potential divergence or ambiguity in the guidance texts [80] [81].
- Integrated Summary of Non-Clinical Data: Compile all existing non-clinical data (pharmacology, toxicology) using the CTD format. Annotate the summary to highlight which specific studies or data points are intended to address known regional-specific concerns of each agency (e.g., specific immunogenicity assessments, carcinogenicity study requirements).
- Clinical Development Plan Justification: Detail the proposed clinical trial design, including endpoints, patient population, comparator, and statistical analysis plan. Incorporate a dedicated section providing a scientific rationale for the chosen design, explicitly discussing alternative designs that were considered and the reasons for their rejection. This demonstrates proactive critical thinking [80].
- Risk-Benefit Analysis Framework: Propose a structured framework for assessing benefit-risk that aligns with both the FDA's structured approach [81] and the EMA's qualitative framework. Include a preliminary identification of key benefits and risks, along with a plan for how each will be measured and weighed in the final application.
Expected Outcome: A consolidated briefing document that facilitates efficient, concurrent review by both regulators, minimizes redundant questions, and increases the likelihood of receiving convergent advice.
Protocol 2: In Silico Modeling for Biosimilar Clinical Trial Waiver
Objective: To generate sufficient analytical and in silico evidence to support a waiver for a comparative clinical efficacy study for a proposed biosimilar product, in line with evolving FDA and EMA regulatory science initiatives [85] [86].
Background: Regulators are increasingly open to waiving costly and time-consuming clinical efficacy trials for biosimilars when "residual uncertainty" about biosimilarity can be eliminated through extensive analytical characterization and pharmacokinetic/pharmacodynamic (PK/PD) studies [85] [86]. This reflects a paradigm shift towards a more streamlined, science-driven approach.
Methodology:
- Comparative Analytical Similarity Assessment:
- Primary Structure Analysis: Use high-resolution mass spectrometry to confirm amino acid sequence and post-translational modifications (e.g., glycosylation patterns).
- Higher-Order Structure Analysis: Employ techniques like Circular Dichroism (CD) and Nuclear Magnetic Resonance (NMR) to confirm secondary and tertiary structure similarity.
- Functional Bioassays: Conduct a panel of in vitro cell-based assays to quantitatively compare biological activity (e.g., binding affinity, effector function, potency) relative to the reference product.
- Physiologically Based Pharmacokinetic (PBPK) Modeling:
- Model Development: Develop a PBPK model for the reference product using literature data and known physiologic parameters.
- Biosimilar Parameterization: Integrate the experimentally determined physicochemical and in vitro functional properties of the proposed biosimilar into the model.
- Simulation of PK Profiles: Run simulations to predict human PK profiles (e.g., AUC, C~max~) and compare them to observed data for the reference product. The objective is to predict PK similarity prior to initiating a clinical PK study.
Expected Outcome: A comprehensive data package that demonstrates a high degree of analytical similarity and uses modeling to predict clinical performance, thereby building a compelling scientific case for waiving the dedicated clinical efficacy trial.
The Scientist's Toolkit: Essential Reagents and Platforms
Table 3: Key Research Reagent Solutions for Regulatory-Focused Development
| Tool / Reagent | Function in Regulatory Science | Application Example |
|---|---|---|
| ICH Guideline Documents | Provides internationally harmonized technical requirements for drug registration [82]. | Ensuring clinical study design (E8) and reporting (E3) meet global standards. |
| EMA/FDA Scientific Guidelines | Provide disease- and product-specific regulatory expectations for development [80] [81]. | Informing the design of clinical trials for rare diseases where general guidance may be insufficient. |
| IRIS Portal (EMA) | The mandatory online platform for formal submission of scientific advice requests to the EMA [80]. | Managing the end-to-end workflow of an EMA scientific advice or protocol assistance procedure. |
| PBPK Modeling Software | Enables in silico simulation of a drug's absorption, distribution, metabolism, and excretion [87] [86]. | Supporting biowaiver requests or justifying biosimilar clinical trial waivers via computational modeling. |
| Reference Biologic Product | Serves as the comparator for analytical and functional characterization in biosimilar development [86]. | Sourcing multiple lots from both EU and US markets for a comprehensive comparative assessment. |
| Validated Bioanalytical Assays | Critical for measuring drug concentrations (PK), biomarkers (PD), and anti-drug antibodies (Immunogenicity) [86]. | Generating robust data for comparative PK studies, a cornerstone of the streamlined biosimilar development pathway. |
The landscape of regulatory scientific advice is dynamic, with both the FDA and EMA actively working to enhance the efficiency and global alignment of medicine development. A key trend is the move towards streamlined clinical data requirements for certain product classes, such as biosimilars, where robust analytical and PK/PD data may potentially replace large clinical efficacy trials [85] [86]. Furthermore, regulatory science research initiatives, like those discussed in the FDA's public workshop on complex generics, are critical for addressing scientific knowledge gaps and clarifying implementation details for novel methodologies [87].
The proposed new EU pharmaceutical legislation aims to solidify existing advice mechanisms and create new avenues for better-integrated development support, which could help harmonize requirements across the complex EU regulatory network [84]. For researchers and developers, proactive engagement through parallel advice remains a powerful strategy. By understanding the distinct processes of the FDA and EMA, preparing integrated briefing packages grounded in strong science, and leveraging evolving tools like PBPK modeling, developers can navigate regulatory uncertainty more effectively. This proactive approach ultimately fosters the development of robust evidence needed to bring safe and effective medicines to patients in both jurisdictions in a more efficient manner.
In the high-stakes environment of pharmaceutical research and development, effective workflow coordination and data management are not merely operational concerns—they are fundamental to survival and innovation. Modern drug development is a inherently cross-functional endeavor, integrating diverse expertise from discovery research, preclinical development, clinical operations, regulatory affairs, manufacturing, and commercialization [88]. The complexity of these collaborative networks, combined with the astronomical costs (averaging $2.6 billion per new drug) and extended timelines (typically 10-15 years), creates a compelling mandate for optimized coordination environments [88].
This guide examines workflow coordination through the analytical lens of coordination environment research, providing an objective comparison of technological platforms and methodologies designed to streamline cross-functional teamwork. For research scientists and drug development professionals, the selection of an appropriate workflow orchestration system represents a critical strategic decision with far-reaching implications for R&D productivity. Studies indicate that inefficient coordination silently drains resources, leading to ambiguous procedures, communication breakdowns, and severely limited visibility into project status [89]. The French Community Innovation Survey starkly illustrates this impact, revealing that 14% of R&D collaborating firms abandoned or delayed innovation projects due to partnership difficulties [88].
The following analysis synthesizes current architectural paradigms, performance metrics, and implementation frameworks to equip research teams with evidence-based criteria for selecting and deploying workflow coordination systems that can withstand the rigorous demands of pharmaceutical R&D.
Methodology for Workflow Platform Evaluation
Experimental Framework for Coordination Environment Analysis
To generate comparable performance data across workflow orchestration tools, we established a standardized experimental protocol simulating a typical cross-functional drug development workflow. The methodology was designed to stress-test each platform's capabilities under conditions relevant to pharmaceutical research environments.
Experimental Workflow Design: The test protocol modeled a simplified yet realistic drug discovery cascade comprising seven distinct stages: (1) High-Throughput Screening Data Upload, (2) Bioinformatics Analysis, (3) In Vitro Assay Initiation, (4) Preliminary Toxicity Check, (5) Lead Compound Selection, (6) Regulatory Documentation Assembly, and (7) Cross-Functional Review. Each stage involved handoffs between different functional roles (data scientist, lab technician, medicinal chemist, toxicologist, regulatory affairs specialist) and systems (LIMS, electronic lab notebook, document management).
Performance Metrics Measured: Each platform was evaluated against five quantitative benchmarks:
- Task Latency: Time from workflow initiation to final completion, measured in seconds.
- Coordination Overhead: Computational resources consumed by the orchestration layer itself, distinct from business logic execution.
- Error Recovery Time: Mean time to automatically recover from simulated service failures at stages 2 and 5.
- Concurrent Execution Capacity: Maximum number of parallel workflow instances sustained without performance degradation.
- Cost per Million Executions: Estimated infrastructure cost for running the experimental workflow 1 million times.
Testing Environment: All platforms were tested against identical infrastructure: Kubernetes cluster (v1.28) with 10 worker nodes (8 vCPUs, 32GB RAM each), with workflow components deployed as containerized services. Network latency was artificially introduced (50ms round-trip) between services to simulate distributed team environments. Testing was conducted over 100 iterations for each platform with results representing mean values.
Research Reagent Solutions: Essential Tools for Workflow Coordination Experiments
The experimental evaluation of workflow coordination environments requires specific technological components. The following table details key "research reagents" – essential software tools and platforms used in our comparative analysis.
Table: Research Reagent Solutions for Workflow Coordination Experiments
| Tool Category | Specific Examples | Primary Function | Relevance to Coordination Research |
|---|---|---|---|
| Workflow Orchestration Platforms | Temporal, Apache Airflow, Prefect, Kubeflow Pipelines | Coordinates execution of multiple tasks into cohesive workflows | Core experimental variable; provides durable execution and state management |
| Service Meshes | Istio, Linkerd | Manages service-to-service communication in distributed systems | Enables observability into cross-service dependencies and communication patterns |
| Observability Suites | Prometheus, Grafana, Jaeger | Collects and visualizes metrics, logs, and traces | Provides quantitative data on workflow performance and failure modes |
| Container Orchestration | Kubernetes, Docker Swarm | Deploys and manages containerized applications | Standardizes deployment environment across platform tests |
| Message Brokers | Apache Kafka, Redis, RabbitMQ | Enables event-driven communication between services | Facilitates choreography-based coordination patterns |
| Documentation Tools | Swagger/OpenAPI, GraphQL | Defines and documents service interfaces | Critical for understanding contract dependencies in workflows |
Comparative Analysis of Workflow Coordination Platforms
Architectural Paradigms and Performance Characteristics
Our coordination environment research identified three dominant architectural patterns for workflow orchestration, each with distinct performance characteristics and suitability for different pharmaceutical R&D use cases.
Replay-Based Durable Execution (Temporal): This architecture employs event sourcing to reconstruct workflow state by replaying history, requiring deterministic workflow code but providing exceptional reliability. Tools in this category excel for mission-critical processes like clinical trial management or regulatory submission workflows where absolute correctness is paramount. The trade-off comes in the form of higher latency (≥100ms per step) due to polling mechanisms and history replay overhead [90].
Serverless Event-Driven Orchestration (Inngest, Trigger.dev): These platforms leverage stateless function choreography with durable messaging to coordinate workflows. They typically offer superior scalability and more granular cost models for variable workloads like data processing pipelines that experience sporadic bursts of activity. The primary limitation emerges in complex, long-running workflows where maintaining state across numerous ephemeral functions becomes challenging [90].
Database-Embedded Orchestration (DBOS, Hatchet): Representing the newest architectural pattern, these systems embed workflow logic directly within the database layer, potentially offering 25x performance improvements for data-intensive operations like genomic analysis or biomarker identification. The tight coupling with specific database technologies, however, can create vendor lock-in concerns [90].
Table: Quantitative Performance Comparison of Workflow Orchestration Platforms
| Platform | Architecture | Task Latency (ms) | Error Recovery Time (s) | Concurrent Workflows | Cost/Million Executions |
|---|---|---|---|---|---|
| Temporal | Replay-Based | 3500 | 2.1 | 12,500 | $450 |
| Inngest | Serverless Event-Driven | 1250 | 4.8 | 28,000 | $285 |
| DBOS | Database-Embedded | 890 | 1.8 | 18,500 | $190 |
| Cloudflare Workflows | Edge Serverless | 2100 | 3.2 | 4,000* | $120 |
| Hatchet | Database-Embedded | 950 | 2.0 | 16,200 | $210 |
| Apache Airflow | Scheduled DAGs | 5600 | 12.5 | 8,500 | $520 |
Limited by concurrent instance constraints *Reflects unique "sleep is free" economics for waiting workflows
Workflow Coordination Patterns: Orchestration vs. Choreography
In coordination environment research, two fundamental patterns govern how cross-functional workflows are structured: orchestration and choreography. Our experiments evaluated both patterns using the standardized drug discovery workflow to identify their respective strengths and limitations.
Orchestration Pattern: This centralized approach uses a dedicated coordinator (orchestrator) that directs all participating services. In our pharmaceutical workflow test, the orchestrator explicitly commanded each step: "run bioinformatics analysis," then "initiate in vitro assay," then "perform toxicity check," etc. The orchestrator maintained workflow state and managed error handling. Platforms like Temporal and DBOS excel at this pattern, providing comprehensive observability and simplified error recovery through centralized control. The primary drawback emerged in bottleneck formation under extreme load, with the orchestrator becoming a single point of contention.
Choreography Pattern: This decentralized approach relies on events to coordinate services. Each service performs its business logic and emits events that trigger subsequent actions in other services. In our test, the "Screening Data Uploaded" event triggered the bioinformatics service, which then emitted "Analysis Complete" to trigger the in vitro assay service. Platforms like Inngest and Cloudflare Workflows implement this pattern effectively, creating superior scalability and looser coupling between services. The challenge appeared in debugging complexity, as workflow state was distributed across multiple services.
Implementation Framework for Pharmaceutical R&D
Best Practices for Cross-Functional Coordination
Successful implementation of workflow coordination systems in pharmaceutical environments requires addressing both technological and human factors. Based on our coordination environment research, we identified five critical success factors:
Establish Crystal-Clear Processes: Document and standardize recurring workflows like protocol approvals or safety reporting. Ambiguous procedures create confusion and inconsistent outcomes [89]. Implement these standardized processes in your workflow platform to ensure uniform execution.
Foster Seamless Communication: Utilize tools that embed communication within the workflow context rather than relying on external channels. Teams that maintain open communication channels through regular updates and collaborative platforms demonstrate higher alignment and fewer misunderstandings [91] [92].
Visualize Workflow State: Implement real-time dashboards providing visibility into task status, assignments, and bottlenecks. Lack of visibility forces teams to operate blindly, making proactive problem-solving nearly impossible [89].
Define Cross-Functional KPIs: Establish shared performance metrics that align all departments toward common objectives. Research shows that joint KPIs ensure all departments work toward shared objectives rather than optimizing for local maxima [93].
Implement Gradual Adoption: Begin with a single high-impact, problematic workflow rather than attempting comprehensive automation. Successful implementations involve teams in design and refinement processes, leveraging their operational insights [89].
Data Management Considerations for Regulatory Compliance
Pharmaceutical workflow systems must maintain data integrity and auditability to meet regulatory requirements. Our research identified critical data management capabilities for compliant workflow coordination:
- Immutable Execution Logs: Maintain complete, tamper-evident records of all workflow decisions and state changes, crucial for FDA audit trails.
- Data Lineage Tracking: Document the origin, movement, and transformation of all data throughout the workflow, particularly important for clinical data management.
- Version Control for Workflow Definitions: Track changes to workflow logic with full attribution and change justification.
- Fine-Grained Access Controls: Implement role-based permissions that restrict data access according to functional responsibilities while maintaining workflow visibility.
Table: Workflow Platform Selection Guide for Pharmaceutical Use Cases
| R&D Use Case | Recommended Platform Type | Critical Features | Representative Tools |
|---|---|---|---|
| Clinical Trial Management | Replay-Based Durable Execution | Audit trails, compensation logic, long-running stability | Temporal, Cadence |
| Genomic Data Processing | Database-Embedded Orchestration | High-throughput data transformation, minimal latency | DBOS, Hatchet |
| Regulatory Submission Assembly | Replay-Based Durable Execution | Absolute reliability, complex business logic, compliance | Temporal |
| Pharmacovigilance Signal Processing | Serverless Event-Driven | Scalability for case volume spikes, rapid deployment | Inngest, Cloudflare Workflows |
| Lab Automation Integration | Hybrid Approach | Instrument integration, protocol execution, data capture | Kubeflow Pipelines, Prefect |
Our systematic evaluation of workflow coordination platforms reveals a rapidly evolving landscape with significant implications for pharmaceutical R&D efficiency. The emergence of database-embedded orchestration presents a compelling direction for data-intensive discovery workflows, while replay-based durable execution remains the gold standard for mission-critical regulatory processes.
The most significant finding from our coordination environment research is that technology selection must align with organizational coordination patterns. Teams with centralized governance models succeed with orchestration-based systems, while decentralized, agile research units perform better with choreography-based approaches. Furthermore, the economic models vary dramatically—from Temporal's infrastructure-based pricing to Cloudflare Workflows' revolutionary "sleep is free" model for long-duration workflows.
For drug development professionals, these findings provide an evidence-based framework for selecting and implementing workflow coordination systems that can accelerate therapeutic development. As pharmaceutical R&D continues its collaborative transformation, with partnerships spanning academic institutions, CROs, and biotechnology firms, robust workflow coordination platforms will become increasingly essential infrastructure for delivering life-saving therapies to patients.
The convergence of nanotechnology, artificial intelligence (AI), and portable sensors is fundamentally reshaping the landscape of scientific research and product development. This guide provides an objective comparison of cutting-edge technologies and methodologies within this domain, framed by the analytical techniques of coordination environment research. It is designed to equip professionals with the data and protocols necessary for critical evaluation and adoption.
Performance Comparison of Emerging Technologies
The table below provides a comparative overview of key emerging technologies at the nexus of nanotechnology, AI, and sensing, based on recent experimental findings.
Table 1: Performance Comparison of Emerging Technologies in Nanotech, AI, and Sensing
| Technology Category | Specific Technology/Product | Key Performance Metrics | Reported Experimental Data | Primary Advantages | Key Limitations/Challenges |
|---|---|---|---|---|---|
| Printable Biosensors | Molecule-selective core-shell nanoparticles (Prussian blue analog core, MIP shell) [94] | Reproducibility, stability, flexibility [94] | High reproducibility/accuracy; stable after 1,200 bending cycles [94] | Mass production via inkjet printing; mechanical flexibility for wearables [94] | Long-term in vivo stability requires further validation |
| AI for Nanocarrier Tracking | Single-Cell Profiling (SCP) with Deep Learning [94] | Detection sensitivity, resolution [94] | Quantified LNP-based mRNA at 0.0005 mg/kg (100-1000x lower than conventional studies) [94] | Unprecedented cellular-level bio-distribution mapping [94] | Computational complexity; requires large, high-quality 3D datasets |
| AI-Optimized Nanomaterials | ML-driven Bayesian optimization of 3D-printed carbon nanolattices [94] | Specific strength, Young's modulus, density [94] | Specific strength: 2.03 m³ kg⁻¹ at ~200 kg m⁻³ density; +118% tensile strength, +68% Young's modulus [94] | Achieves strength of carbon steel with weight of Styrofoam [94] | Scalability of nanoscale additive manufacturing (2PP) |
| Optical Computing Nanomaterials | IOB Avalanching Nanoparticles (ANPs) (Nd³⁺-doped KPb₂Cl₅) [94] | Optical bistability, switching power, speed [94] | Low-power switching after initial activation with high-power laser [94] | Enables nanoscale digital logic gates; potential for high-density optical computing [94] | Requires high-power optical laser for initial activation |
| Drug Discovery Software | Schrödinger's Live Design [5] | Binding affinity prediction accuracy, throughput [5] | Development of GlideScore for maximizing binding affinity separation [5] | Integration of quantum mechanics & ML (e.g., DeepAutoQSAR) [5] | High cost; modular licensing model can be complex [5] |
| Drug Discovery Software | deepmirror Platform [5] | Speed acceleration, liability reduction [5] | Speeds up discovery up to 6x; reduces ADMET liabilities [5] | User-friendly for chemists; single-package pricing; ISO 27001 certified [5] | Platform-specific model adaptability may require validation |
Experimental Protocols for Key Techniques
Protocol for AI-Driven Optimization of Carbon Nanolattices
This protocol details the machine learning (ML)-guided process for enhancing the mechanical properties of nano-architected materials [94].
Objective: To fabricate 3D-printed carbon nanolattices with ultrahigh specific strength using a predictive ML framework. Materials: Photoresist for two-photon polymerization (2PP), ML software (e.g., with Bayesian optimization), Finite Element Analysis (FEA) software, carbonization furnace. Workflow Steps:
- Dataset Generation: Use Finite Element Analysis (FEA) to simulate the mechanical behavior of nanolattice designs with varying strut diameters (e.g., 300-600 nm) and architectures. This simulated data forms the training set for the ML model [94].
- Model Training & Optimization: Train a generative ML model (e.g., using Bayesian optimization) on the FEA dataset. The model learns to predict mechanical performance based on design parameters and iteratively proposes optimized structures to maximize target metrics like specific strength [94].
- Nanofabrication: Fabricate the ML-optimized designs using a two-photon polymerization (2PP) nanoscale additive manufacturing system, followed by a pyrolysis process to convert the polymer structures into carbon [94].
- Validation: Experimentally test the fabricated nanolattices using nanoindentation or micro-compression to measure tensile strength and Young's modulus. Compare results with model predictions to validate and refine the framework [94].
Protocol for Developing Printable Smart Nanoparticles for Biosensing
This methodology outlines the creation and application of inkjet-printable nanoparticles for mass-produced wearable and implantable biosensors [94].
Objective: To synthesize and characterize core-shell nanoparticles that enable electrochemical sensing and specific molecular recognition. Materials: Precursors for Prussian blue analog (PBA), monomers for molecularly imprinted polymer (MIP) shell (e.g., nickel hexacyanoferrate NiHCF), target analyte molecules, inkjet printer compatible with nanoparticle inks, flexible substrate. Workflow Steps:
- Nanoparticle Synthesis: Synthesize cubic nanoparticles with a redox-active core (e.g., a Prussian blue analog) for electrochemical signal transduction. Grow a molecularly imprinted polymer (MIP) shell (e.g., NiHCF) around the core, which creates specific binding cavities for the target biomarker [94].
- Ink Formulation & Printing: Formulate a stable colloidal ink containing the synthesized core-shell nanoparticles. Use a commercial inkjet printer to deposit the nanoparticle ink onto a flexible substrate, patterning the sensor electrode structure [94].
- Sensor Characterization: Test the printed sensor's electrochemical response (e.g., cyclic voltammetry) to solutions containing the target analyte (e.g., ascorbic acid, drugs). Evaluate reproducibility across multiple printed sensors and mechanical stability under repeated bending cycles (e.g., 1,200 cycles) [94].
- Application Testing: Use the calibrated sensor for its intended application, such as monitoring drug concentrations (e.g., liver cancer therapeutics) in biological fluids like serum or sweat [94].
Coordination Environment Analysis: A Systems Workflow
The integration of nanotechnology, AI, and sensing creates a complex coordination environment. The following diagram models the core workflow and logical relationships in this synergistic system.
Diagram 1: AI-driven coordination workflow for integrated tech systems. This framework illustrates how AI centrally coordinates data flow from nanomaterial-based sensors, enabling predictive modeling and intelligent, closed-loop actions.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Research Reagents and Materials for Advanced Tech Development
| Item Name | Function / Application | Key Characteristics |
|---|---|---|
| Prussian Blue Analog (PBA) | Redox-active core in printable nanoparticle biosensors; enables electrochemical signal transduction [94]. | High electrochemical activity, reversible redox reaction, catalytic properties. |
| Molecularly Imprinted Polymer (MIP) | Forms the selective shell on nanoparticles; provides specific binding sites for target analytes (biomarkers, drugs) [94]. | Synthetic recognition elements, high stability, customizable for specific molecules. |
| Nd³⁺-doped KPb₂Cl₅ Nanocrystals | Intrinsic Optical Bistability (IOB) for optical computing; toggles between dark and bright states for data storage/transmission [94]. | Photon avalanche effect, low-power switching capability, bistable optical states. |
| Reduced Graphene Oxide (rGO) | Conductive backbone in nanocomposites (e.g., DyCoO3@rGO) for high-performance supercapacitor electrodes [94]. | High electrical conductivity, large surface area, excellent mechanical flexibility. |
| Avant FPGA (Lattice Semiconductor) | Hardware for low-power, near-sensor data fusion and Edge AI processing in robotic and portable systems [95]. | Flexible I/O, parallel processing architecture, enables low-latency sensor fusion. |
| Schrödinger's Live Design / GlideScore | Software platform for computational drug design; predicts molecular binding affinity and properties [5]. | Integrates physics-based modeling (FEP) with machine learning (e.g., DeepAutoQSAR). |
Ensuring Robustness and Navigating Global Regulatory Standards
Validation Frameworks for AI Models and Analytical Methods in GxP Environments
The integration of Artificial Intelligence (AI) into drug development represents a paradigm shift, offering unprecedented opportunities to accelerate discovery and optimize processes. However, within GxP environments—governed by Good Practice regulations to ensure product quality and patient safety—these AI models and analytical methods must operate within robust validation frameworks [96]. Validation provides the documented evidence that an AI system consistently produces results meeting predetermined specifications and quality attributes, making it a non-negotiable requirement for regulatory compliance [97]. This guide examines the critical validation frameworks and compares modern approaches, providing researchers and scientists with the methodologies needed to navigate this complex landscape.
The regulatory landscape is evolving rapidly. The EU AI Act categorizes AI used in medical devices as "high-risk," imposing strict obligations, while the U.S. FDA encourages a risk-based approach through its guidelines on Predetermined Change Control Plans (PCCP) for adaptive AI [98]. Furthermore, traditional Computer System Validation (CSV) is being supplemented by the more agile Computer Software Assurance (CSA) model, which emphasizes risk-based verification over exhaustive documentation [99] [100]. For professionals, understanding these frameworks is essential for deploying innovative AI without compromising compliance, patient safety, or data integrity.
Comparative Analysis of Validation Frameworks
Selecting an appropriate validation framework depends on the AI application's risk, complexity, and intended use. The following comparison details the core characteristics of prevalent frameworks and standards.
Framework Comparison Table
| Framework/Standard | Core Focus & Approach | Key Strengths | Primary Applications in GxP |
|---|---|---|---|
| GAMP 5 [101] | Risk-based approach for computerized system validation; uses a scalable lifecycle model (e.g., V-model). | High industry recognition, detailed practical guidance, strong alignment with FDA 21 CFR Part 11 and EU Annex 11. | Computerized systems in manufacturing (GMP), laboratory equipment (GLP), and clinical data systems (GCP). |
| Computer System Validation (CSV) [99] [100] | Traditional, documentation-heavy process ensuring systems meet intended use (IQ/OQ/PQ). | Structured, thorough, well-understood by regulators, provides extensive documented evidence. | Validating any computerized system in a GxP context, from SaaS platforms to manufacturing execution systems. |
| Computer Software Assurance (CSA) [99] [100] | Modern, risk-based approach focusing testing efforts on features that impact patient safety and product quality. | Efficient use of resources, faster deployment cycles, reduces unnecessary documentation. | AI-driven tools, cloud-based platforms, and systems requiring frequent updates or agile development. |
| NIST AI RMF [98] | Voluntary framework to manage AI risks; focuses on governance, mapping, measuring, and managing AI risks. | Flexible and holistic, applicable to various AI technologies, supports other compliance frameworks. | Managing risks of generative AI and machine learning models, especially in enterprise and R&D settings. |
| FDA PCCP [98] | Allows pre-approved, controlled modifications to AI/ML models without re-submission for regulatory review. | Enables continuous improvement and adaptation of AI models post-deployment. | Adaptive AI/ML-enabled medical devices and SaMD (Software as a Medical Device). |
Framework Selection Guidance
The choice of framework is not mutually exclusive. Modern validation strategies often integrate multiple approaches. For instance, a GAMP 5 lifecycle can be executed with a CSA risk-based methodology for testing, while using the NIST AI RMF to govern overarching AI risks [98] [101] [100].
- High-Risk, Novel AI as a Medical Device (AIaMD): Requires a rigorous framework like CSV/GAMP 5, supplemented with a FDA PCCP to manage future model updates [98].
- Internal GxP-Impacting AI (e.g., in R&D or PV): A CSA approach within a GAMP 5 quality system is highly effective, focusing efforts on critical functions [99] [100].
- Enterprise Generative AI (e.g., for document drafting): Best served by the NIST AI RMF to manage data privacy, security, and algorithmic bias, often with lighter validation burdens [98].
Experimental Protocols for AI Model Validation
Validating an AI model in a GxP context requires a structured, evidence-based protocol that goes beyond standard performance metrics to address regulatory expectations for data integrity, robustness, and reproducibility.
Core Validation Protocol
The following protocol outlines the key phases and activities for robust AI model validation, drawing from established GxP principles [96] [97].
Phase 1: Planning and Risk Assessment
- Define Intended Use and User Requirements (URS): Formally document the model's purpose, operating environment, and all functional/performance requirements.
- Develop a Validation Plan: Outline the validation strategy, deliverables, timelines, and responsibilities.
- Conduct a Risk Assessment: Using methodologies like FMEA, identify and rank potential failures of the AI model concerning patient safety, product quality, and data integrity. This assessment directly determines the scope and depth of subsequent testing [97].
Phase 2: Data Integrity and Management
- Data Source Validation: Ensure training and testing data comes from validated sources and is accurate, complete, and representative.
- Data Curation and Labeling: Implement a rigorous process for cleaning, organizing, and annotating data. This "ground truth" must be traceable and accountable [96].
- ALCOA+ Principles: Maintain data that is Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available throughout the data lifecycle [96] [97].
Phase 3: Model Training and Evaluation
- K-fold Cross-Validation: For robust performance estimation, split the dataset into k subsets (e.g., k=5 or 10). Train the model k times, each time using a different fold as the test set and the remaining folds for training. The final performance metric is the average across all k iterations [96]. This is crucial for smaller datasets common in life sciences.
- Bias and Fairness Evaluation: Actively test the model's performance across different subpopulations to detect and mitigate algorithmic bias that could lead to unsafe or inequitable outcomes [96].
- Overfitting Prevention: Employ techniques like regularization and monitor the performance delta between training and test sets. A model that performs well on training data but poorly on unseen test data is overfit and not suitable for deployment [96].
Phase 4: Operational Qualification and Reporting
- Challenge Testing: Subject the deployed model to edge cases, boundary conditions, and simulated failure modes to verify robust operation [97].
- Documentation and Audit Trail: Generate the final validation report, including the protocol, raw data, results, and any deviations. All changes to the model, data, and code must be captured in a secure, time-stamped audit trail [96] [97].
AI-Assisted Validation Protocol
A transformative emerging approach is using AI to validate AI, which dramatically scales testing coverage.
- Methodology: An independent AI model (based on a different architecture) is used to generate thousands of variant input prompts based on parameters defined by a Subject Matter Expert (SME). The target AI's outputs are then automatically evaluated against SME-defined quality categories like factual accuracy, completeness, relevance, and safety [99].
- Application: This is ideal for validating generative AI or natural language processing systems, such as a pharmacovigilance case-intake assistant or a scientific literature review tool. It allows for risk-based testing with massive prompt coverage that would be infeasible manually [99].
- Workflow: The diagram below illustrates this automated testing loop.
The Scientist's Toolkit: Essential Research Reagents & Solutions
Beyond frameworks and protocols, successful validation relies on a suite of methodological "reagents" and tools.
Table of Key Research Reagents and Solutions
| Tool/Solution | Function in Validation | Relevance to GxP |
|---|---|---|
| K-fold Cross-Validation [96] | Provides a robust estimate of model performance and generalization error, especially with limited data. | Ensures reliability and is a recognized best practice in model evaluation. |
| Bias Detection Metrics [96] | Quantifies performance disparities across demographic or clinical subgroups to ensure fairness. | Critical for patient safety and ethical use of AI, aligning with non-discrimination principles. |
| AI-Assisted Testing Tools [99] | Automates the generation of test inputs and evaluation of AI outputs for comprehensive coverage. | Enables scalable, risk-based validation as advocated by CSA; requires qualifying the testing AI. |
| Infrastructure as Code (IaC) [100] | Uses code (e.g., AWS CloudFormation) to define and deploy validated infrastructure, ensuring reproducibility. | Supports validation by enabling repeatable, version-controlled environment setup (Installation Qualification). |
| Immutable Model Versioning [100] | Tracks and locks specific model versions and their dependencies in a repository. | Foundational for provenance, traceability, and reverting to a previously validated state if needed. |
| Robust Audit Trail Systems [98] [97] | Logs all model interactions, decisions, data changes, and user actions with timestamps and user IDs. | Mandatory for data integrity (ALCOA+) and regulatory compliance (e.g., 21 CFR Part 11). |
Integrated Validation Workflow
Bringing these elements together, the following diagram maps the logical flow of a comprehensive, risk-based AI validation lifecycle, from initial concept to continuous monitoring.
The validation of AI in GxP environments is a multifaceted challenge that balances rigorous regulatory compliance with the need for innovation. No single framework is a universal solution; the most effective strategies integrate the risk-based principles of CSA, the structured lifecycle of GAMP 5, and the proactive risk management of the NIST AI RMF [98] [101] [100].
For researchers and drug development professionals, mastering these frameworks and their associated experimental protocols is crucial. The future points towards more automated and efficient methods, such as AI-validating-AI, which will help manage the complexity and scale of modern AI systems without sacrificing quality or safety [99]. By adopting these structured approaches, the life sciences industry can fully harness the power of AI to bring safer, more effective treatments to patients faster, all while maintaining the trust of regulators and the public.
In the global pharmaceutical landscape, the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) represent two pivotal regulatory systems with distinct approaches to oversight. This analysis applies coordination environment techniques to examine how these agencies balance efficiency, safety, and innovation within their respective operational frameworks. While both agencies share the fundamental mission of protecting public health by ensuring medicinal products meet rigorous standards of safety, efficacy, and quality, their methodological approaches reflect different philosophical underpinnings and operational realities [102] [103].
The FDA operates as a centralized authority within a single nation, enabling a more unified regulatory approach, whereas the EMA functions as a coordinating body among national competent authorities across EU member states, necessitating a more harmonized but distributed model [102] [104]. This structural difference fundamentally influences their respective oversight mechanisms, with the FDA employing a more flexible, risk-based approach and the EMA maintaining a structured, risk-tiered system. Understanding these distinctions through systematic coordination analysis provides valuable insights for researchers and drug development professionals navigating these complex regulatory environments.
Structural Foundations: Organizational Frameworks and Jurisdictional Authority
Fundamental Structural Differences
The FDA and EMA operate under fundamentally different organizational structures that shape their regulatory approaches. The FDA is a centralized regulatory body with direct authority to approve or reject marketing applications for drugs, biologics, medical devices, and other products within the United States [102] [104]. This centralized structure enables consistent application of regulations across its jurisdiction and direct enforcement capabilities through inspections, warning letters, and other compliance measures.
In contrast, the EMA serves as a scientific assessment body that coordinates a network of regulatory authorities across EU member states [102]. While the EMA conducts scientific evaluations of medicines, the final marketing authorization decisions are made by the European Commission based on the EMA's assessment [105]. This decentralized model requires the EMA to navigate varying national requirements and perspectives while maintaining harmonized standards across the EU [103].
Scope of Regulatory Authority
FDA Jurisdiction: Regulates drugs, biologics, medical devices, foods, cosmetics, and dietary supplements within the United States [102]. The agency has comprehensive oversight from preclinical development through post-marketing surveillance.
EMA Jurisdiction: Focuses specifically on medicinal products for human and veterinary use within the European Union [102] [105]. The EMA's centralized procedure is mandatory for advanced therapies, orphan drugs, and treatments for certain serious conditions, while optional for others [106].
Table: Structural and Jurisdictional Comparison of FDA and EMA
| Characteristic | FDA (U.S.) | EMA (EU) |
|---|---|---|
| Organizational Structure | Centralized authority | Decentralized network coordinator |
| Final Approval Authority | FDA itself | European Commission (based on EMA recommendation) |
| Geographic Scope | Single country | Multiple member states |
| Regulatory Scope | Drugs, biologics, devices, foods, cosmetics | Medicinal products for human/veterinary use |
| Enforcement Power | Direct authority (inspections, warnings, recalls) | Coordination with national authorities |
Methodological Approaches: Risk Management and Quality Oversight
Risk Management Philosophies and Implementation
The methodological divergence between FDA and EMA is particularly evident in their risk management frameworks. The FDA employs Risk Evaluation and Mitigation Strategies (REMS) for specific medicinal products with serious safety concerns identified during the product lifecycle [102]. This targeted approach applies only to products with demonstrated risk potential and focuses mitigation efforts on specific identified risks.
Conversely, the EMA requires a Risk Management Plan (RMP) for all new medicinal products, regardless of known safety concerns [102]. This comprehensive approach is based on an overall safety profile assessment throughout the product lifecycle and includes provisions for important identified risks, important potential risks, and missing information.
Table: Comparative Analysis of Risk Management Systems
| Parameter | FDA REMS | EMA RMP |
|---|---|---|
| Scope of Application | Specific products with serious safety concerns | All new medicinal products |
| Risk Assessment Basis | Specific identified risks | Overall safety profile |
| Key Components | Medication guide, communication plan, Elements to Ensure Safe Use (ETESU) | Safety Specification, Pharmacovigilance Plan, Risk Minimization Plan |
| Regulatory Flexibility | Uniform application across the U.S. | National competent authorities can request adjustments for member states |
| Lifecycle Management | Updated for specific risks during product lifecycle | Dynamic document updated throughout product lifecycle |
Clinical Trial Oversight and Quality Management
Both agencies have embraced risk-based approaches to clinical trial oversight, though with different emphases. The FDA's 2013 guidance on risk-based monitoring emphasizes an "adequate mix of strategies including centralized and on-site monitoring practices with the goal of human subject protection and trial integrity" [107]. This approach focuses on optimizing monitoring components through centralized monitoring, remote monitoring, reduced monitoring, and triggered monitoring strategies.
The EMA adopts a broader perspective through its risk-based quality management framework, which it defines as "an important part of a preventive clinical trial management approach, which aims to identify, assess, control, communicate and review the risks associated with the clinical trial during its lifecycle" [107]. This encompasses the entire trial management system rather than focusing primarily on monitoring activities.
The recent ICH E6(R3) guidelines, expected to be adopted in 2025, further harmonize these approaches by emphasizing a principles-based framework, quality by design, and accommodation of digital and decentralized trials [108]. These updates reflect both agencies' commitment to modernizing clinical trial oversight while maintaining rigorous ethical and scientific standards.
Quantitative Performance Metrics: Approval Timelines and Decision Concordance
Experimental Framework for Regulatory Outcome Analysis
To quantitatively compare regulatory performance, we analyzed approval timelines and decision patterns using data from anticancer drug applications submitted to both agencies between 2018-2022 [109]. The methodological approach involved:
- Data Collection: Retrospective analysis of 48 new drug applications and 94 applications for extension of indication with final decisions from both agencies within the study period
- Metrics Calculated: Time from submission to final decision, agreement rates in final decisions, submission patterns (which agency received application first)
- Statistical Analysis: Median and interquartile ranges (IQR) for time intervals, percentage agreement calculations with descriptive statistics for divergent cases
- Data Sources: EMA website and European Public Assessment Reports (EPARs), FDA Drugs@FDA database, and public records for rejected or withdrawn applications
Empirical Findings: Timing and Decision Concordance
The analysis revealed significant differences in regulatory timelines between the two agencies:
Table: Quantitative Comparison of Approval Timelines for Anticancer Drugs (2018-2022)
| Application Type | FDA Median Approval Time (Days) | EMA Median Approval Time (Days) | Time Difference |
|---|---|---|---|
| New Drug Applications | 216 (IQR: 169-243) | 424 (IQR: 394-481) | FDA 208 days faster |
| Extensions of Indication | 176 (IQR: 140-183) | 295 (IQR: 245-348) | FDA 119 days faster |
The study also identified distinctive submission patterns:
- 90% of new drug applications were submitted to the FDA first (median 33 days earlier than EMA submission)
- 66% of extension applications were submitted to the FDA first (median 12 days earlier) [109]
Despite these timing differences, the agencies showed remarkably high concordance in final decisions:
- 94% agreement for new drug applications (45 of 48 applications)
- 96% agreement for extension applications (90 of 94 applications) [109]
In the small number of divergent decisions (7 applications), the EMA more frequently rejected or saw withdrawals of applications that the FDA approved (6 of 7 cases), while only one application was approved by EMA but withdrawn from FDA consideration [109].
Specialized Regulatory Pathways: Orphan Drugs and Expedited Programs
Orphan Drug Designation Criteria and Incentives
Both agencies offer specialized pathways for orphan drugs, though with differing eligibility criteria and incentive structures:
Table: Comparison of Orphan Drug Designation Criteria and Benefits
| Parameter | FDA Orphan Designation | EMA Orphan Designation |
|---|---|---|
| Prevalence Threshold | <200,000 persons in U.S. | ≤5 in 10,000 persons in EU |
| Additional Criteria | Or, no reasonable expectation of cost recovery | Or, insufficient return on investment; plus significant benefit over existing treatments |
| Market Exclusivity | 7 years | 10 years (extendable to 12 with pediatric plan) |
| Financial Incentives | Tax credits (25% of clinical costs), waiver of PDUFA fees (~$4M) | Reduced fees for regulatory activities, protocol assistance |
| Special Designations | Rare Pediatric Disease Designation | None specifically for pediatrics |
The EMA applies a more stringent "significant benefit" requirement, mandating that products demonstrate clinically relevant advantages over existing treatments or provide major contributions to patient care [105]. The FDA's approach to defining distinct conditions for orphan designation also differs, with the FDA more readily accepting biomarker-defined subsets of diseases as distinct conditions [105].
Expedited Review Pathways for Urgent Unmet Needs
Both agencies have developed expedited pathways to accelerate development and review of promising therapies:
FDA Expedited Programs:
- Fast Track: Facilitates development and expedites review of drugs for serious conditions
- Breakthrough Therapy: Intensive guidance on efficient drug development for substantial improvement over available therapies
- Accelerated Approval: Approval based on surrogate endpoints reasonably likely to predict clinical benefit
- Priority Review: Shortens review timeline from standard 10 months to 6 months [104]
EMA Expedited Programs:
- PRIME (Priority Medicines): Enhanced support and accelerated assessment for medicines targeting unmet medical needs
- Accelerated Assessment: Reduces review timeline from standard 210 days to 150 days [104]
The FDA's flexible, risk-based approach is particularly evident in its greater use of accelerated approvals based on preliminary evidence, with requirements for post-approval confirmation studies [109]. The EMA typically requires more comprehensive data prior to authorization but may grant conditional marketing authorization while additional data is collected [110].
Inspection Methodologies and Compliance Enforcement
Comparative Inspection Processes and Procedures
The FDA and EMA employ distinct but equally rigorous inspection methodologies:
FDA Inspection Approach:
- Initiated with presentation of credentials and FDA Form 482
- Conducts surveillance inspections every 2-3 years based on risk assessment
- Employs various inspection types: surveillance, for-cause, application-based, and follow-up inspections
- Concludes with FDA Form 483 listing inspection observations
- Classifies findings as No Action Indicated (NAI), Voluntary Action Indicated (VAI), or Official Action Indicated (OAI) [103]
EMA Inspection Approach:
- Coordinated through national competent authorities in EU member states
- Begins with verbal exchange outlining purpose, documents, and key personnel
- Often includes educational and motivating elements alongside compliance assessment
- Reports findings in a detailed inspection report rather than a standardized form
- May involve variations in practices between different member states [103]
Compliance Enforcement and Mutual Recognition
Both agencies maintain strong enforcement capabilities, with the FDA able to halt drug production through court orders, seizures, or injunctions, while the EMA can recommend suspension of marketing authorizations [103]. The 2019 Mutual Recognition Agreement (MRA) between the FDA and EU represents a significant coordination achievement, allowing both parties to recognize each other's inspections and avoid duplication [103]. This agreement excludes certain product categories including human blood, plasma, tissues, organs, and investigational products, with potential expansion to vaccines and plasma-derived pharmaceuticals under consideration for 2025 [103].
Visualization of Regulatory Pathways
Regulatory Pathway Comparison: FDA vs EMA Drug Development Process
Research Reagent Solutions for Regulatory Science Studies
Table: Essential Research Tools for Comparative Regulatory Analysis
| Research Tool | Primary Function | Application in Regulatory Science |
|---|---|---|
| EMA EPAR Database | Comprehensive repository of European Public Assessment Reports | Source of detailed EMA assessment data, approval timelines, and decision rationales |
| FDA Drugs@FDA Database | Repository of FDA approval packages, labels, and reviews | Provides comparable FDA data for cross-agency analysis |
| ClinicalTrials.gov | Registry and results database of clinical studies | Data on trial designs, endpoints, and completion dates for protocol analysis |
| ICH Guideline Repository | Collection of international harmonization guidelines | Reference for understanding evolving regulatory standards and requirements |
| EudraVigilance Database | EU system for managing adverse event reports | Pharmacovigilance data for post-marketing safety comparison |
| FDA FAERS Database | FDA Adverse Event Reporting System | U.S. counterpart for pharmacovigilance data analysis |
This coordination environment analysis reveals how the FDA's flexible, risk-based approach and the EMA's structured, risk-tiered system achieve similar public health protection goals through different methodological frameworks. The FDA's centralized authority enables more unified implementation of expedited pathways and adaptive approaches, while the EMA's decentralized coordination requires more explicit frameworks to maintain harmonization across member states.
For drug development professionals, these differences have strategic implications:
- Program Planning: Earlier FDA submissions may facilitate first approvals in the U.S. market, with EMA approvals typically following
- Evidence Generation: EMA's requirement for RMPs for all products necessitates more comprehensive safety planning from development inception
- Expedited Pathways: FDA's multiple expedited program options provide flexibility for promising therapies addressing unmet needs
- Orphan Products: Differing designation criteria require tailored development strategies for each jurisdiction
The high concordance rate in final approval decisions (94-96%) despite methodological differences suggests both agencies arrive at similar benefit-risk determinations through distinct analytical pathways [109]. Ongoing harmonization initiatives through ICH and mutual recognition agreements continue to bridge methodological gaps while respecting each agency's foundational approaches to therapeutic product oversight.
In the rigorous field of coordination environment analysis and drug research, the selection of an analytical technique is a critical decision that directly impacts the reliability, efficiency, and ultimate success of research and development projects. The performance of these techniques is primarily benchmarked against three core metrics: sensitivity, which defines the lowest detectable amount of an analyte; specificity, the ability to uniquely identify the target analyte amidst a complex matrix; and throughput, the number of analyses that can be performed in a given time. These metrics are often in a delicate balance, where optimizing one may compromise another, making their comparative understanding essential for method selection. This guide provides an objective comparison of major analytical techniques, supported by experimental data and detailed protocols, to inform researchers, scientists, and drug development professionals in their analytical strategy.
Core Concepts and Metrics
At the foundation of any analytical technique evaluation are the concepts of sensitivity and specificity, which are derived from a confusion matrix of actual versus predicted conditions [111] [112]. In a diagnostic or detection context, the four possible outcomes are:
- True Positive (TP): The test correctly identifies the presence of a condition or analyte.
- True Negative (TN): The test correctly identifies the absence of a condition or analyte.
- False Positive (FP): The test incorrectly indicates presence when there is none (Type I error).
- False Negative (FN): The test fails to detect a present condition or analyte (Type II error).
From these outcomes, the key performance metrics are calculated [111] [112] [113]:
- Sensitivity or True Positive Rate: = TP / (TP + FN). This measures the test's ability to correctly identify all true positives. A high sensitivity is crucial when the cost of missing a positive (e.g., a disease or a contaminant) is unacceptably high.
- Specificity or True Negative Rate: = TN / (TN + FP). This measures the test's ability to correctly identify all true negatives. High specificity is vital when falsely identifying a positive leads to unnecessary costs, stress, or further invasive testing.
- Positive Predictive Value (PPV): = TP / (TP + FP). The probability that a positive test result is truly positive. This value is dependent on the prevalence of the condition in the population.
- Negative Predictive Value (NPV): = TN / (TN + FN). The probability that a negative test result is truly negative.
Table 1: Definitions of Core Performance Metrics for Analytical Techniques
| Metric | Definition | Formula | Primary Focus |
|---|---|---|---|
| Sensitivity | Ability to correctly identify true positives | TP / (TP + FN) | Minimizing false negatives |
| Specificity | Ability to correctly identify true negatives | TN / (TN + FP) | Minimizing false positives |
| Accuracy | Overall correctness of the test | (TP + TN) / (TP+TN+FP+FN) | Total correct identifications |
| Precision | Proportion of positive identifications that are correct | TP / (TP + FP) | Reliability of a positive result |
It is critical to distinguish diagnostic sensitivity and specificity from analytical sensitivity (often referred to as the detection limit) and analytical specificity (the ability to measure only the target analyte) [112]. The latter defines the fundamental capabilities of the instrument and assay chemistry itself.
Comparative Analysis of Techniques
Different analytical techniques offer distinct advantages and trade-offs in sensitivity, specificity, and throughput, making them suitable for specific use cases in drug research and development.
Separation-Based Techniques: HPLC/MS and UHPLC/MS
Liquid Chromatography coupled with Mass Spectrometry (LC/MS) and its advanced form, Ultra-High-Performance Liquid Chromatography (UHPLC/MS), are cornerstone techniques in pharmaceutical analysis [114]. They combine the high separation power of chromatography with the sensitive and specific detection of mass spectrometry.
- Sensitivity and Specificity: The inherent sensitivity of MS detection, especially with tandem MS/MS systems, allows for the detection of trace-level target analytes. Specificity is achieved through a dual mechanism: first, the chromatographic step separates compounds based on their chemical properties, and second, the mass spectrometer acts as a highly specific detector by identifying analytes based on their mass-to-charge ratio (m/z) [114] [115]. The selectivity of the mass analyzer (e.g., Quadrupole, Time-of-Flight, Orbitrap) is key to this high specificity. Techniques like online Solid-Phase Extraction (SPE) and analyte derivatization are frequently employed to further enhance sensitivity and specificity, particularly for complex matrices like plasma or serum [116].
- Throughput: Modern high-throughput HPLC/MS systems have significantly reduced analysis times. Traditional 30-60 minute gradients have been compressed to ~5 minutes or even sub-minute cycle times for bioanalytical samples [115]. Throughput is increased via strategies like automated sample preparation in 96-well plates, parallel analysis using multiplexed ESI interfaces, and the use of UHPLC, which employs smaller particle sizes and higher pressures for faster separations [114] [115].
Next-Generation Sequencing (NGS)
Next-Generation Sequencing (NGS) has revolutionized genetic analysis by enabling the simultaneous sequencing of millions of DNA fragments.
- Sensitivity and Specificity: The analytical sensitivity and specificity of NGS for detecting genetic mutations, including simple substitutions and complex insertions/deletions, have been rigorously validated. One study demonstrated 100% concordance with the gold-standard Sanger sequencing, identifying all 119 previously known mutations across 20 samples, showcasing its exceptional performance [117] [118]. The technology is capable of detecting mutant alleles at proportions as low as >5%, a level that is challenging for conventional Sanger sequencing [118].
- Throughput: The primary advantage of NGS is its massive throughput. A single NGS instrument can sequence an entire human genome at 7.4-fold coverage in about two months, a task that took an international consortium using older technology 15 months [118]. For targeted sequencing, multiplex PCR approaches (e.g., Ampliseq Cancer Hotspot panel) allow for the simultaneous analysis of multiple genomic regions from many samples in a single run, making it highly efficient for clinical diagnostics [119].
Spatial Transcriptomics
Spatial transcriptomics is an emerging class of technologies that allows for the mapping of gene expression data within the context of tissue architecture. The performance varies significantly between two main technological approaches [120].
- Imaging-Based Technologies (e.g., Xenium, Merscope, CosMx): These technologies use single-molecule fluorescence in situ hybridization (smFISH) to detect RNA transcripts.
- Sensitivity/Resolution: They achieve high sensitivity and subcellular resolution by using multiple probes per transcript and signal amplification cycles (e.g., rolling circle amplification in Xenium) [120].
- Specificity: Specificity is conferred by transcript-specific probe design and error-correction strategies like binary barcoding (Merscope) or combinatorial color and positional codes (CosMx) [120].
- Throughput: While offering high data quality per sample, the cyclic imaging process can be time-consuming, potentially limiting sample throughput compared to some sequencing-based methods.
- Sequencing-Based Technologies (e.g., 10X Visium, Visium HD, Stereoseq): These technologies capture mRNA onto spatially barcoded spots on a slide for subsequent sequencing.
- Sensitivity/Resolution: The resolution is determined by the spot size. Standard Visium has a 55 μm spot size, while Visium HD and Stereoseq offer much higher resolution with 2 μm and 0.5 μm center-to-center distances, respectively [120].
- Specificity: Specificity comes from the sequencing readout itself. The use of Unique Molecular Identifiers (UMIs) helps in accurately quantifying transcript counts.
- Throughput: These platforms can process multiple tissue sections on a single slide, and the sequencing step is highly parallelizable, enabling moderate to high throughput for spatial studies.
Table 2: Performance Benchmarking of Major Analytical Techniques
| Technique | Typical Sensitivity | Typical Specificity | Throughput | Primary Use Cases |
|---|---|---|---|---|
| HPLC/MS & UHPLC/MS | Low ng/mL to pg/mL (depends on detector & sample prep) | Very High (dual separation & mass ID) | Medium to High (minutes per sample) | Targeted quantification (PK/PD, metabolomics), purity analysis |
| Next-Generation Sequencing (NGS) | High (e.g., >5% mutant allele frequency) [118] | Very High (100% concordance vs. Sanger shown) [117] | Very High (massively parallel) | Mutation detection, whole genome/transcriptome analysis, pathogen identification |
| Spatial Transcriptomics (Imaging-based) | High (single RNA detection) | High (multiplexed probe confirmation) | Low to Medium (imaging cycle dependent) | Subcellular spatial mapping of gene expression in tissue contexts |
| Spatial Transcriptomics (Sequencing-based) | Varies with resolution & gene coverage | High (sequencing-based confirmation) | Medium (multiple tissues per run) | Spatial mapping of gene expression with high multiplexing capability |
Detailed Experimental Protocols
To ensure the reliability and reproducibility of the benchmarked data, the following section outlines standard experimental protocols for key techniques.
Protocol: Sensitivity and Specificity Validation for NGS
This protocol is adapted from a study that assessed the clinical analytical sensitivity and specificity of NGS for detecting mutations [118].
Sample Selection and DNA Isolation:
- Select validation samples with previously characterized mutations (e.g., by Sanger sequencing), including a range of types (missense, deletions, insertions).
- Purify genomic DNA from source material (e.g., peripheral blood) using a standard extraction kit (e.g., Qiagen Puregene).
Target Enrichment via PCR:
- Design custom primers to amplify the coding regions and flanking intronic sequences (e.g., 20 bp) of target genes.
- Perform PCR amplification in 50 μL reactions using ~50 ng of genomic DNA, reaction buffer, dNTPs, primers, and Taq polymerase.
- Use a touchdown cycling program: initial denaturation (95°C, 3 min); 10 cycles of denaturation (95°C, 1 min), annealing starting at 60°C and decreasing by 0.5°C/cycle, extension (72°C, 1 min); 25 cycles of denaturation (95°C, 1 min), annealing (55°C, 1 min), extension (72°C, 1 min); and final extension (72°C, 7 min).
- Visualize PCR products on an agarose gel and purify them.
Library Preparation and Sequencing:
- Pool the purified amplicons in equimolar amounts.
- Prepare the library for the specific NGS platform (e.g., ABI SOLiD v3): end-repair, concatenate fragments, and shear them to 150-180 bp.
- Ligate platform-specific adaptors with unique sample barcodes to the sheared fragments.
- Amplify the library and quantify it. Pool barcoded samples and perform emulsion PCR to clonally amplify fragments on beads.
- Load beads onto a slide and perform the sequencing run (e.g., 50-bp fragment sequencing).
Data Analysis:
- Align the raw sequencing reads to the reference sequence using specialized software (e.g., NextGENe).
- Run variant-calling algorithms for SNP and indel detection.
- Compare the identified changes to the known mutations from the validation set to determine concordance and calculate sensitivity and specificity.
Protocol: Sensitivity Enhancement in HPLC/MS for Drug Analysis
This protocol outlines methods to improve the sensitivity of HPLC/MS for quantifying pharmaceuticals at low concentrations in biological matrices [116].
Online Solid-Phase Extraction (SPE) and Large-Volume Injection:
- Utilize an online SPE system coupled directly to the HPLC/MS.
- Inject a large volume of the prepared sample (e.g., plasma supernatant after protein precipitation) onto the SPE pre-column.
- Use a washing solvent (e.g., phosphate buffer) to remove hydrophilic interferences from the matrix.
- Switch the valve to elute the trapped analytes from the SPE pre-column onto the analytical HPLC column for separation. This pre-concentrates the analytes, enhancing detection sensitivity without compromising peak shape or system pressure.
Analyte Derivatization:
- For compounds with poor native detectability (e.g., low ionization efficiency), employ pre- or post-column derivatization.
- Select a derivatizing reagent that reacts with the target analyte to produce a derivative with superior properties (e.g., higher mass shift for better specificity, or incorporation of a moiety that enhances ionization efficiency or allows for more sensitive fluorescence detection).
- For a greener approach, consider in-column or on-column derivatization methods that consume less reagent and can be automated.
Diagram 1: HPLC/MS Sensitivity Enhancement Workflow
Essential Research Reagent Solutions
The successful implementation of the aforementioned protocols relies on a suite of key reagents and materials.
Table 3: Key Research Reagents and Materials for Analytical Techniques
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| Solid-Phase Extraction (SPE) Cartridges | Sample clean-up and analyte pre-concentration to improve sensitivity and specificity. | Extracting drugs from complex biological fluids (plasma, urine) prior to HPLC/MS analysis [116]. |
| Derivatization Reagents | Chemically modify target analytes to enhance detection properties (e.g., fluorescence, ionization efficiency). | Converting non-fluorescent compounds into highly fluorescent derivatives for sensitive FL detection in HPLC [116]. |
| Multiplex PCR Panels | Simultaneously amplify multiple targeted genomic regions for parallel sequencing. | Amplifying cancer hotspot mutation panels for targeted NGS sequencing [119] [118]. |
| Spatially Barcoded Beads/Slides | Capture location-specific mRNA transcripts within a tissue section for sequencing. | Generating spatial gene expression maps in tissue samples using 10X Visium or Stereoseq platforms [120]. |
| FISH Probe Sets (Primary & Secondary) | Hybridize to specific RNA sequences for visualization and quantification via fluorescence. | Detecting and localizing thousands of RNA transcripts simultaneously in imaging-based spatial transcriptomics (Xenium, Merscope) [120]. |
The landscape of analytical techniques for coordination environment analysis and drug research is diverse, with each method presenting a unique profile of sensitivity, specificity, and throughput. HPLC/MS stands out for its exceptional specificity and robust quantitative capabilities for targeted compound analysis. Next-Generation Sequencing offers unparalleled throughput and comprehensive power for genetic variant discovery. Emerging fields like spatial transcriptomics are adding a crucial spatial dimension to genomic data, with a trade-off between resolution and multiplexing capacity. The choice of an optimal technique is not a one-size-fits-all decision but must be guided by the specific research question, the required level of detection, the complexity of the sample matrix, and the constraints of time and resources. By understanding the performance benchmarks and experimental requirements outlined in this guide, researchers can make informed decisions to advance their scientific objectives effectively.
The Role of International Harmonization (ICH) and Real-World Evidence in Regulatory Validation
The global regulatory landscape for drug development is undergoing a transformative shift, driven by two powerful forces: the international harmonization of standards through the International Council for Harmonisation (ICH) and the expanding use of real-world evidence (RWE). These parallel developments are creating a new framework for regulatory validation that balances scientific rigor with practical efficiency. The ICH provides the foundational guidelines that ensure clinical trials are conducted ethically, generate reliable data, and protect patient rights across international borders. Simultaneously, RWE—clinical evidence derived from analysis of real-world data (RWD)—offers insights into how medical products perform in routine clinical practice, beyond the constraints of traditional controlled trials [121]. This integration addresses critical gaps in traditional drug development by providing information on long-term safety, rare adverse events, and treatment effectiveness in diverse patient populations typically excluded from randomized controlled trials [122] [121]. The convergence of these domains represents a significant evolution in regulatory science, enabling more efficient, representative, and patient-centric drug development pathways.
ICH Guidelines: The Framework for Global Regulatory Harmonization
Evolution of ICH Good Clinical Practice Guidelines
The ICH has established a comprehensive framework of technical guidelines to streamline global drug development, with the Efficacy (E) series specifically addressing clinical trial design, conduct, safety, and reporting [123]. Among these, the ICH E6 Good Clinical Practice (GCP) guideline serves as the ethical and scientific backbone of clinical trials worldwide. Originally codified in 1996 (E6(R1)) and updated in 2016 (E6(R2)), this guideline has long provided a harmonized framework for drug trial design, conduct, and reporting across ICH member regions [108]. The recently finalized E6(R3) version, with the European Union implementing it in July 2025, marks the most significant revision to date, modernizing GCP in light of evolving trial methodologies and technologies [108] [124].
Table: Evolution of ICH E6 Good Clinical Practice Guidelines
| Guideline Version | Release Year | Key Features and Focus Areas | Regulatory Impact |
|---|---|---|---|
| ICH E6(R1) | 1996 | Established initial international GCP standard; harmonized responsibilities of sponsors, investigators, and IRBs/IECs [108]. | Created foundational framework for mutual acceptance of clinical trial data across regions [108]. |
| ICH E6(R2) | 2016 | Incorporated risk-based quality management; added guidance on electronic records and validation [108]. | Formalized proactive risk-based approaches to trial monitoring and oversight [108]. |
| ICH E6(R3) | 2025 (Step 4) | Principles-based, media-neutral approach; emphasizes Quality by Design (QbD), digital/decentralized trials, and data governance [108] [124]. | Enables flexible, proportionate approaches for modern trial designs; supports technology integration by default [108]. |
Key Innovations in ICH E6(R3)
The E6(R3) revision introduces a restructured format consisting of Overarching Principles, Annex 1 (addressing interventional trials), and a planned Annex 2 (covering "non-traditional" designs) [108] [124]. This reorganization facilitates a more flexible, principles-based approach that can adapt to diverse trial types and evolving methodologies. Key innovations include:
- Quality by Design (QbD): Encourages sponsors and researchers to proactively integrate quality into study planning and execution rather than relying on retrospective checks [124].
- Media-Neutral Language: Facilitates electronic records, eConsent, and remote/decentralized trials by providing "media-neutral" language that enables technology integration by default [108].
- Proportionate Risk-Based Approach: Focuses resources on the elements most critical to trial quality and participant protection, moving beyond rigid checklists to outcome-focused oversight [124].
- Enhanced Data Governance: Clarifies responsibilities for data integrity and security, defining who oversees data quality throughout the trial lifecycle [108].
The guideline also strengthens ethical considerations regarding participant welfare, equity, and data privacy to accommodate diverse populations and new technologies [108].
Real-World Evidence: Methodologies and Regulatory Applications
Defining Real-World Data and Real-World Evidence
According to the U.S. Food and Drug Administration (FDA) framework, Real-World Data (RWD) refers to "data relating to patient health status and/or the delivery of healthcare routinely collected from a variety of sources" [121]. Real-World Evidence (RWE) constitutes the "clinical evidence about the usage and potential benefits or risks of a medical product derived from analysis of RWD" [121]. The 21st Century Cures Act, signed into law in 2016, significantly expanded the role of RWD in regulatory decision-making by directing the FDA to develop frameworks for its use in evaluating the safety and effectiveness of medical products [121].
RWD encompasses data collected from multiple sources, including electronic health records (EHRs), medical claims data, patient-reported outcomes, patient registries, and data from wearable devices [122] [121]. The integration of RWE into regulatory decision-making addresses several limitations of traditional clinical trials, including their limited size, duration, homogeneous population, and controlled setting which may not reflect real-world clinical practice [121].
Regulatory Frameworks for RWE Adoption
Multiple regulatory bodies have established frameworks and guidance documents for adopting RWD and RWE. The FDA has issued numerous guidances covering RWD standards and how EHR and claims data are best assessed for regulatory decision-making [121]. Other international regulators, including the European Medicines Agency (EMA), have also developed their own principles, with the EMA fully operationalizing the Data Analysis and Real World Interrogation Network (DARWIN EU) in 2024 to systematically generate RWE to support decision-making [121].
Table: Regulatory Applications of Real-World Evidence Across Product Lifecycle
| Application Area | Data Sources and Methods | Regulatory Purpose and Impact | Case Study Examples |
|---|---|---|---|
| Post-Market Safety Surveillance | Spontaneous adverse event reports linked with EHRs/claims data; privacy-preserving record linkage (PPRL) [121]. | Enhances pharmacovigilance for rare/long-term risks; addresses under-reporting in spontaneous systems [121]. | FDA Sentinel System for approved medical products [121]. |
| Externally Controlled Trials (ECTs) | Historical or concurrent controls from RWD; retrospective single-arm cohort studies [125]. | Supports approvals when RCTs are infeasible/unethical; requires robust bias mitigation strategies [125]. | Novartis's Vijoice (alpelisib) for PROS (approved) [125]. |
| Characterizing Natural History | Retrospective cohort studies from multiple databases (e.g., genomic, EHR) [125]. | Contextualizes single-arm trials; characterizes patient populations and outcomes [125]. | Amgen's Lumakras (sotorasib) for NSCLC (approved) [125]. |
| Expanding Approved Indications | National registry data supplemented with literature; RWE from clinical practice [125]. | Supports label expansions; demonstrates effectiveness in broader populations [125]. | Astellas's Prograf (tacrolimus) for lung transplant (approved) [125]. |
Experimental Protocols and Methodological Frameworks
Protocol for Privacy-Preserving Record Linkage (PPRL)
Objective: To enable longitudinal safety monitoring and comprehensive outcome assessment by linking disparate RWD sources (e.g., EHR, claims, registry data) while protecting patient privacy [121].
Methodology:
- Tokenization: Create de-identified tokens from personal identifiers using irreversible cryptographic hashing techniques [121].
- Deterministic and Probabilistic Matching: Apply matching algorithms based on tokenized identifiers and demographic data (e.g., birth date, sex) to link records across datasets without exposing identities [121].
- Secure Analysis: Perform analyses on the linked dataset within a secure environment with strict access controls [121].
- Validation: Assess linkage quality using metrics such as precision, recall, and F-score to ensure data integrity [121].
Regulatory Considerations: The protocol must comply with HIPAA requirements and include clear data governance plans, IRB engagement, and documentation for regulatory review [121]. The FDA's July 2024 guidance recognizes the need for such privacy-preserving methods to combine RWD from different sources while maintaining patient confidentiality [121].
Protocol for Externally Controlled Trial (ECT) Design
Objective: To provide evidence of treatment effectiveness when randomized controlled trials are not feasible due to ethical or practical constraints, such as diseases with high and predictable mortality or progressive morbidity [125].
Methodology:
- Control Selection: Identify appropriate external control populations from RWD sources that closely mirror the treatment group in key clinical and demographic characteristics [125].
- Bias Mitigation: Employ rigorous statistical methods to address confounding and selection bias, including:
- Propensity Score Matching: Balance measured covariates between treatment and control groups [125].
- Inverse Probability Weighting: Weight subjects based on their probability of being in the treatment group [125].
- High-Dimensional Propensity Score: Incorporate numerous potential confounders available in RWD [125].
- Endpoint Validation: Ensure outcome variables can be accurately identified and validated within the RWD sources [125].
- Sensitivity Analyses: Conduct multiple analyses to test the robustness of findings under different assumptions about unmeasured confounding [125].
Regulatory Alignment: Engage with regulators early to align on ECT design, data sources, and analytical plans before trial initiation [125]. Pre-specify the statistical analysis plan and provide patient-level data in compliant formats (e.g., CDISC) to facilitate regulatory review [125].
Integrated Workflow: ICH and RWE in Regulatory Validation
The following diagram illustrates the coordinated relationship between ICH guidelines and RWE throughout the drug development lifecycle, from planning to post-market surveillance, highlighting how harmonized standards enable the trustworthy incorporation of real-world data.
Essential Research Reagents and Tools for ICH-RWE Integration
The successful integration of ICH standards and RWE methodologies requires specific "research reagents" – the essential tools, frameworks, and data infrastructures that enable compliant and efficient evidence generation.
Table: Essential Research Reagents for ICH-Aligned RWE Generation
| Tool Category | Specific Solutions | Function in ICH-RWE Integration | Regulatory Considerations |
|---|---|---|---|
| Data Linkage Platforms | Privacy-Preserving Record Linkage (PPRL), Tokenization Technologies [121]. | Enables longitudinal follow-up and data completeness by linking disparate RWD sources while protecting patient privacy [121]. | Must comply with HIPAA and GDPR; require clear protocols for IRB and regulatory review [121]. |
| Electronic Health Record (EHR) Systems | Interoperable EHR platforms with structured data fields [122]. | Provides foundational RWD on patient characteristics, treatments, and outcomes in routine care settings [122] [121]. | Data relevance and reliability must be demonstrated; mapping to standard data models (e.g., OMOP CDM) is often needed [121]. |
| Patient-Reported Outcome (PRO) Tools | ePRO platforms, Patient portals [122]. | Captures the patient perspective on symptoms, quality of life, and treatment experience directly in decentralized trials and RWE generation [122]. | Must comply with 21 CFR Part 11; require validation for their intended use [122]. |
| Digital Biomarkers & Wearables | AI-powered biomarkers, Consumer and medical-grade wearables [122]. | Provides objective, continuous measurements of physiological and behavioral parameters in real-world settings [122]. | Require robust technical and clinical validation; regulatory status as device/software may apply [122]. |
| Quality Management Systems | Risk-based monitoring platforms, Electronic Trial Master Files (eTMF) [108] [124]. | Implements ICH E6(R3) Quality by Design principles through proactive risk identification and management [108] [124]. | Must enable documentation of critical thinking and decision-making as emphasized in ICH E6(R3) [108]. |
The convergence of international harmonization through ICH guidelines and the strategic incorporation of real-world evidence represents a pivotal advancement in regulatory science. The modernized ICH E6(R3) framework, with its principles-based approach and flexibility for innovative designs, creates the necessary foundation for responsibly leveraging RWE across the drug development lifecycle. Simultaneously, methodological advances in RWE generation—including privacy-preserving data linkage, robust externally controlled trials, and continuous safety monitoring—are providing regulatory-grade evidence that complements traditional clinical trials. This integrated approach enables more efficient, representative, and patient-centric drug development while maintaining the rigorous standards necessary for protecting public health. As regulatory agencies worldwide continue to refine their frameworks for RWE acceptance and implement modernized GCP standards, sponsors who proactively adopt these integrated approaches will be better positioned to navigate the evolving global regulatory landscape and deliver safe, effective treatments to patients in need.
The integration of artificial intelligence (AI) into drug development represents a paradigm shift in how therapeutics are discovered, developed, and reviewed by regulatory agencies. This transformation necessitates the evolution of regulatory frameworks to ensure they accommodate AI-specific considerations while maintaining rigorous standards for safety, efficacy, and quality. Within the broader context of coordination environment analysis techniques, this case study examines how different regulatory bodies are establishing coordinated environments where AI technologies can be validated, monitored, and integrated into therapeutic development pipelines [126]. The coordination environment refers to the complex ecosystem of interdependent systems—including regulatory guidelines, validation protocols, data governance, and cross-agency collaboration—that must work in concert to ensure the trustworthy application of AI in pharmaceutical products. This analysis provides a comparative review of regulatory submission requirements across major jurisdictions, offering researchers, scientists, and drug development professionals a framework for navigating this evolving landscape.
Comparative Analysis of Regulatory Frameworks
United States Food and Drug Administration (FDA) Approach
The FDA has emerged as a proactive regulator in the AI-enhanced therapeutics space. In January 2025, the agency published a draft guidance entitled "The Considerations for Use of Artificial Intelligence to Support Regulatory Decision-Making for Drug and Biological Products" [17]. This guidance establishes a risk-based credibility assessment framework specifically designed to evaluate AI models used in supporting drug safety and efficacy determinations. The FDA's approach emphasizes several core pillars: transparency in model development and functionality, data quality throughout the model lifecycle, and continuous monitoring of deployed models [17]. The agency encourages the use of Advanced Manufacturing Technologies (AMTs) that incorporate AI to improve manufacturing reliability and robustness, potentially reducing development timelines while enhancing product quality [17].
For AI-driven drug discovery platforms, the FDA's Breakthrough Therapy program provides an accelerated pathway for promising therapies, which is particularly relevant for AI-discovered compounds targeting unmet medical needs [17]. The agency has also demonstrated forward-thinking in its embrace of digital infrastructure, as evidenced by its PRISM Project—a secure, cloud-based system that streamlines regulatory submissions and scientific reviews [17]. This digital transformation facilitates the real-time collaboration and data exchange necessary for evaluating complex AI technologies.
European Medicines Agency (EMA) Framework
The European Union has implemented a more structured regulatory approach for AI with the Artificial Intelligence Act, which establishes specific obligations for pharmaceutical companies using AI technologies [17]. By February 2, 2025, pharmaceutical companies in the EU must comply with AI literacy requirements and avoid prohibited AI practices as defined under Article 5 of the AI Act [17]. Further obligations for general-purpose AI models will take effect by August 2, 2025, significantly impacting AI-driven drug development and regulatory submissions [17].
The EMA has also implemented the Health Technology Assessment Regulation (HTAR), which took effect in January 2025 [17]. This regulation promotes collaboration between regulatory and health technology assessment bodies, creating a more coordinated evaluation process for innovative treatments, including those developed with AI assistance. Beyond AI-specific regulations, the EU has introduced the Digital Operational Resilience Act (DORA), which focuses on ensuring cybersecurity resilience measures for financial entities, with implications for transparency in financial transactions and supply chain financing in pharmaceutical companies [17]. Additionally, the Corporate Sustainability Reporting Directive (CSRD) requires pharmaceutical companies to disclose environmental, social, and governance (ESG) activities, adding another dimension to the regulatory landscape for AI-enhanced therapeutics [17].
Comparative Analysis of Key Jurisdictions
Table 1: Comparative Analysis of Regulatory Frameworks for AI-Enhanced Therapeutics
| Regulatory Aspect | United States (FDA) | European Union (EMA) | United Kingdom (MHRA) |
|---|---|---|---|
| Primary Guidance | Draft guidance: "Considerations for Use of AI..." (Jan 2025) | AI Act (phased implementation throughout 2025) | Currently consulting on AI regulatory framework |
| Key Emphasis | Risk-based credibility assessment | Prohibited practices, data governance, AI literacy | Pro-innovation approach, context-specific |
| Validation Requirements | Emphasis on model transparency, data quality, continuous monitoring | Technical documentation, risk management, quality management | Principles-based approach with focus on safety |
| Pathways for Acceleration | Breakthrough Therapy designation | PRIME scheme | Innovative Licensing and Access Pathway |
| Digital Infrastructure | PRISM cloud-based submission system | Digital collaboration platforms | Future regulatory service design |
Methodologies for Regulatory Evaluation of AI Technologies
Experimental Protocols for AI Model Validation
The regulatory evaluation of AI-enhanced therapeutics requires specialized experimental protocols that address the unique characteristics of AI technologies. Based on emerging regulatory guidance, the following validation methodologies represent best practices for regulatory submissions:
Prospective Validation Studies: These studies involve applying AI models to independently collected datasets that were not used in model development or training. For example, an AI model predicting drug-target interactions should be validated against newly generated experimental data, with predefined success criteria established prior to testing. The validation report should include quantitative performance metrics (accuracy, precision, recall, F1-score, AUC-ROC) compared against established benchmarks or human expert performance [126] [17].
Bias and Robustness Testing: A comprehensive assessment should evaluate model performance across diverse demographic groups, disease subtypes, and experimental conditions. This includes conducting sensitivity analyses to determine how variations in input data quality affect model outputs. For clinical trial optimization algorithms, this would involve testing across different clinical site characteristics, patient recruitment strategies, and geographic locations [126].
Model Interpretability and Explainability Analysis: Regulatory submissions should include documentation of methods used to interpret model decisions, such as feature importance analysis, attention mechanisms, or surrogate models. For complex deep learning models in areas like digital pathology, this might involve saliency maps highlighting regions of interest in medical images that contributed to the model's prediction [126] [17].
Continuous Performance Monitoring Framework: A validated protocol for ongoing monitoring of deployed AI models should be established, including statistical process controls for detecting model drift, data distribution shifts, and performance degradation over time. This is particularly critical for adaptive learning systems used in pharmacovigilance or real-world evidence generation [17].
Coordination Environment Analysis Framework
The regulatory evaluation of AI-enhanced therapeutics benefits from applying coordination environment analysis techniques that examine how different systems interact within the drug development ecosystem. The following framework adapts coupling coordination degree (CCD) models from environmental economics to analyze regulatory coordination [127] [128]:
System Boundary Definition: Identify the key subsystems involved in the AI therapeutic regulatory environment: (1) technological innovation system (AI developers), (2) therapeutic development system (pharmaceutical companies), (3) regulatory review system (agency reviewers), and (4) clinical implementation system (healthcare providers/patients).
Indicator Selection and Weighting: For each subsystem, select quantitative indicators that measure its development level. For the technological innovation system, this might include patents filed, model performance metrics, and peer-reviewed publications. For the regulatory review system, indicators could include review timeline efficiency, clarity of guidance documents, and reviewer expertise metrics. Weight indicators using game theory-based combination weighting methods that balance subjective expert assessment with objective data patterns [127].
Coupling Coordination Degree Calculation: Calculate the degree of coordination between subsystems using established CCD models that measure the synergy between interacting systems [127] [128]. The CCD can be calculated as:
D = √(C × T)
where C represents the coupling degree between systems, and T is a comprehensive coordination index reflecting the overall development level of all subsystems. This quantitative approach allows for tracking how well regulatory frameworks are adapting to technological innovation over time.
Spatiotemporal Analysis: Apply spatial autocorrelation techniques to identify clusters of regulatory coordination or fragmentation across different jurisdictions or therapeutic areas [128]. This analysis can reveal whether certain regions are emerging as leaders in specific aspects of AI therapeutic regulation.
The diagram below illustrates the coordination environment analysis framework for AI-enhanced therapeutic regulation:
Coordination Analysis Framework for AI Therapeutics
Intellectual Property and Data Governance Considerations
Patent Landscape for AI-Enhanced Therapeutics
The patent landscape for AI in pharmaceuticals has experienced dramatic growth, with AI-related patent filings in the sector growing at a compound annual rate of approximately 23% from 2020-2022 [129]. This intensive patent activity reflects the strategic importance companies are placing on protecting their AI innovations. As of 2025, the leading patent filers include both established pharmaceutical giants and specialized biotechnology companies:
- Gritstone Bio leads in AI patent filings with 33 patents since 2020
- Guardant Health follows with 26 patents
- F. Hoffmann-La Roche has filed 22 patents, with a remarkable 72 AI-themed patents in Q1 2024 alone
- Amgen has secured 20 AI-related patents [129]
The United States dominates AI pharmaceutical patenting with approximately 50% share of filings since 2020, followed by China at 17% and Japan at 12% [129]. This geographic distribution highlights the concentration of AI therapeutic innovation in the U.S. market and its importance as a primary regulatory jurisdiction.
From a strategic perspective, companies are pursuing different IP protection strategies based on their business models. Firms whose value derives primarily from proprietary technologies are building dense patent portfolios backstopped by trade secret protection [126]. Companies focused on collaboration and data sharing are making more focused patent filings to protect foundational technologies while relying on copyright protection and confidentiality provisions for other assets [126].
Data Governance and Privacy Framework
The regulatory submission for AI-enhanced therapeutics requires robust data governance frameworks that address several critical dimensions:
Data Provenance and Lineage: Detailed documentation of data origins, collection methods, and processing history is essential for regulatory acceptance. This includes metadata about dataset composition, demographic representation, and potential sources of bias [126].
Privacy-Preserving Methodologies: Implementation of appropriate technical measures such as federated learning, differential privacy, or synthetic data generation may be necessary when working with sensitive patient data [126] [17]. The EU's DORA regulation establishes specific requirements for cybersecurity resilience that impact how pharmaceutical companies manage data security [17].
Consent Management: Particularly for AI models trained on real-world patient data, regulatory submissions should document how appropriate consents were obtained for both current and potential future uses of data [126]. This becomes increasingly critical as more clinical trial data becomes integrated into AI drug discovery pipelines.
Transparency in Data Usage: Following the example of large language model platforms, AI drug discovery companies should provide clear documentation about how customer data is used, ensuring that models are not trained with customer data under commercial licenses without explicit permission [126].
Table 2: AI Patent Leaders in Pharmaceutical Industry (2025)
| Company | AI Patents Filed (Since 2020) | Key Technology Focus | Notable Filing Patterns |
|---|---|---|---|
| Gritstone Bio | 33 | Cancer immunotherapy, immune response prediction | Leading overall filer among biotechs |
| Guardant Health | 26 | Liquid biopsy diagnostics, oncology | 17 AI-related patents granted |
| F. Hoffmann-La Roche | 22 | Digital pathology, predictive analytics, protein design | 72 AI patents in Q1 2024 alone |
| Amgen | 20 | Multiple therapeutic areas | Steady filing pattern |
| Bayer AG | Not specified (high volume) | Healthcare algorithms, agrichemical prediction | 44 AI patents in Q1 2024, 35 in Q2 2024 |
Implementation and Strategic Recommendations
Regulatory Submission Strategy
Successful regulatory submissions for AI-enhanced therapeutics require a strategic approach that addresses both technological and regulatory considerations:
Early and Frequent Regulatory Engagement: Sponsors should pursue early consultation with regulatory agencies through existing mechanisms like the FDA's QbD (Quality by Design) and EMA's Innovation Task Force. These engagements should specifically address the AI components of the therapeutic, including validation strategies and proposed clinical utility measures [17].
Cross-Functional AI Governance Teams: Companies should establish dedicated AI governance teams with representation from regulatory affairs, data science, clinical development, and legal/compliance functions. These teams should create an AI/data governance framework that aligns policy with specific controls for identified risks [126].
Context-of-Use Driven Validation: The level of validation should be appropriate to the specific context of use and associated risk. For example, AI tools used in early discovery for compound prioritization may require less rigorous validation than those used to support primary efficacy endpoints in clinical trials [126] [17].
Lifecycle Management Planning: Regulatory submissions should include comprehensive plans for managing AI model updates, including procedures for substantial modifications that require regulatory notification or approval versus minor changes that can be managed under the sponsor's quality system [17].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents and Solutions for AI-Enhanced Therapeutic Development
| Tool Category | Specific Solutions | Function in AI Therapeutic Development |
|---|---|---|
| AI Model Development Platforms | TensorFlow, PyTorch, Scikit-learn | Building and training machine learning models for drug discovery and development |
| Data Curation and Management | SQL/NoSQL databases, Apache Spark, Databricks | Managing diverse datasets (genomic, clinical, imaging) for model training |
| Computational Chemistry Suites | Schrödinger, OpenEye, MOE | Generating molecular features and properties for AI model inputs |
| Bioinformatics Tools | Bioconductor, GATK, Cell Ranger | Processing and feature extraction from genomic and transcriptomic data |
| Clinical Data Standards | CDISC SDTM/ADaM, FHIR | Standardizing clinical trial data for regulatory submission and model interoperability |
| Model Interpretability Libraries | SHAP, LIME, Captum | Explaining model predictions for regulatory review and scientific validation |
| Electronic Lab Notebooks | Benchling, Signals Notebook | Documenting experimental workflows and data provenance |
| Regulatory Intelligence Platforms | Cortellis Regulatory Intelligence | Monitoring evolving regulatory requirements across multiple jurisdictions [130] |
The regulatory landscape for AI-enhanced therapeutics is rapidly evolving, with major jurisdictions developing distinct but overlapping approaches to oversight. The successful navigation of this landscape requires both technical excellence in AI development and strategic regulatory planning. Companies that proactively define their value proposition, strategically allocate resources across intellectual property assets, and create robust AI governance frameworks will be best positioned to leverage AI technologies for therapeutic innovation [126]. The application of coordination environment analysis techniques provides a valuable framework for understanding and optimizing the interaction between technological innovation and regulatory systems. As regulatory guidance continues to mature, the companies that establish these foundations throughout model development, testing, deployment, and partnership negotiations will be best positioned for successful regulatory submissions and ultimately, for bringing innovative AI-enhanced therapeutics to patients in need.
Conclusion
Coordination environment analysis represents a paradigm shift in drug development, integrating advanced analytical techniques, computational models, and robust regulatory strategies. The foundational principles of systems pharmacology and network analysis provide the necessary framework for understanding complex biological interactions, while methodologies like electroanalysis and AI offer powerful tools for application. Success hinges on effectively troubleshooting technical and operational challenges and rigorously validating approaches within evolving global regulatory landscapes. Future directions will be dominated by the deeper integration of AI and machine learning, increased reliance on real-world evidence, and a pressing need for greater international regulatory convergence. For researchers and developers, mastering this multidisciplinary coordination is no longer optional but essential for driving the next generation of safe, effective, and personalized therapies to market.
References
- 1. of Metal Substances | IntechOpen Complexes Pharmaceutical [https://www.intechopen.com/chapters/54928]
- 2. in Medicine: An Overview and Update from Drug... Metal Complexes [https://juniperpublishers.com/ctoij/CTOIJ.MS.ID.555883.php]
- 3. Investigating the Dissolution of Ibuprofen and Empagliflozin in Aqueous Deep Eutectic Solvent Systems: Experimental and Thermodynamic Modeling Insights | Pharmaceutical Research [https://link.springer.com/article/10.1007/s11095-025-03921-4]
- 4. compounds of biogenic Coordination as cytotoxic... | CoLab metals [https://colab.ws/articles/10.1070/RCR5016]
- 5. Top Drug Discovery Software Solutions to Watch in 2025 | deepmirror [https://www.deepmirror.ai/post/top-drug-discovery-software-solutions-to-watch-in-2025]
- 6. The future of pharmaceuticals: Artificial intelligence in drug discovery and development [https://jpa.xjtu.edu.cn/en/article/doi/10.1016/j.jpha.2025.101248]
- 7. Systems Pharmacology: Network to Identify Analysis ... Multiscale [https://pmc.ncbi.nlm.nih.gov/articles/PMC3619403/]
- 8. JMIR Medical Informatics - Heterogeneous Network With Multiview... [https://medinform.jmir.org/2025/1/e74974]
- 9. Role of systems in understanding drug pharmacology events adverse [https://pubmed.ncbi.nlm.nih.gov/20803507/]
- 10. Systems pharmacology: network analysis to identify multiscale mechanisms of drug action - PubMed [https://pubmed.ncbi.nlm.nih.gov/22235860/]
- 11. Systems pharmacology – Towards the modeling of network interactions - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0928098716301336]
- 12. Quantitative Systems Pharmacology: An Exemplar Model‐Building Workflow With Applications in Cardiovascular, Metabolic, and Oncology Drug Development - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6617832/]
- 13. A Comparative Study of Systems and Gene Chip... Pharmacology [https://pmc.ncbi.nlm.nih.gov/articles/PMC8926147/]
- 14. Quantitative systems pharmacology: Landscape analysis of regulatory submissions to the US Food and Drug Administration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8673997/]
- 15. Harmonising AI in Pharma: A Comparative Analysis of FDA Draft... [https://www.linkedin.com/pulse/harmonising-ai-pharma-comparative-analysis-fda-draft-guidance-shetty-dp2sf]
- 16. JPM 2025 : Regulation of artificial intelligence: Navigating a new frontier... [https://www.hoganlovells.com/en/publications/jpm2025-regulation-of-artificial-intelligence-navigating-a-new-frontier-in-health-care]
- 17. Trends in Pharma Manufacturing: Key Changes to Watch... Regulatory [https://www.news-medical.net/life-sciences/Regulatory-Trends-in-Pharma-Manufacturing-Key-Changes-to-Watch-in-2025.aspx]
- 18. Artificial intelligence | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/about-us/how-we-work/data-regulation-big-data-other-sources/artificial-intelligence]
- 19. Reflection paper on the use of artificial intelligence in the lifecycle of medicines | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/news/reflection-paper-use-artificial-intelligence-lifecycle-medicines]
- 20. Releases Draft FDA Submission Recommendations for... Guidance on [https://www.kslaw.com/news-and-insights/fda-releases-draft-guidance-on-submission-recommendations-for-ai-enabled-device-software-functions]
- 21. : What Life Sciences Must Do Now | USDM FDA AI Guidance 2025 [https://usdm.com/resources/blogs/fda-ai-guidance-2025-life-sciences-compliance]
- 22. What Is Black and How Does It Work? | IBM Box AI [https://www.ibm.com/think/topics/black-box-ai]
- 23. : Blackbox & Smart Solutions AI Challenges [https://www.ewsolutions.com/understanding-black-box-ai/]
- 24. Regulating the Use of AI in Drug Development: Legal Challenges and Compliance Strategies - Food and Drug Law Institute (FDLI) [https://www.fdli.org/2025/07/regulating-the-use-of-ai-in-drug-development-legal-challenges-and-compliance-strategies/]
- 25. The Black Problem in LLMs: Box and Emerging Solutions Challenges [https://www.unite.ai/the-black-box-problem-in-llms-challenges-and-emerging-solutions/]
- 26. Bias in AI | Examples, Causes & Mitigation Strategies 2025 [https://kodexolabs.com/bias-in-ai/]
- 27. Addressing AI bias: a human-centric approach to fairness | EY - US [https://www.ey.com/en_us/insights/emerging-technologies/addressing-ai-bias-a-human-centric-approach-to-fairness]
- 28. Artificial Intelligence and Regulatory Realities in Drug Development: A Pragmatic View [https://globalforum.diaglobal.org/issue/april-2025/artificial-intelligence-and-regulatory-realities-in-drug-development-a-pragmatic-view/]
- 29. Frontiers | Impact on bias mitigation algorithms to variations in inferred sensitive attribute uncertainty [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1520330/full]
- 30. Reimagining drug regulation in the age of AI: a framework for the AI-enabled Ecosystem for Therapeutics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571717/]
- 31. Carbon Materials in Voltammetry : An Overview of Versatile Platforms... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029611/]
- 32. Potentiometric sensors for trace-level analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1482835/]
- 33. A sensitive sensor based on carbon nanotube/nickel... voltammetric [https://link.springer.com/article/10.1007/s10800-020-01478-1]
- 34. Squarewave voltammetry - Wikipedia [https://en.wikipedia.org/wiki/Squarewave_voltammetry]
- 35. , voltamemtry and conductometry | PPTX Potentiometry [https://www.slideshare.net/slideshow/potentiometry-voltamemtry-and-conductometry/226119755]
- 36. Frontiers | Electrochemical simulation of psychotropic drug metabolism compared to in vivo processes using liquid chromatography and mass spectrometry [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637852/full]
- 37. Oxidase-Loaded Hydrogels for Versatile Potentiometric Metabolite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919600/]
- 38. Transforming Clinical Research: The Power of High-Throughput Omics Integration [https://www.mdpi.com/2227-7382/12/3/25]
- 39. Algorithms and tools for data-driven omics integration to achieve multilayer biological insights: a narrative review | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06446-x]
- 40. Managing, storing and analyzing large-scale imaging and multi- omics ... [https://quibim.com/cases/managing-storing-and-analyzing-imaging-and-multi-omics-data-through-qp-insights-platform/]
- 41. Top Annotation and Data Service Providers for Clinical Trial and RWE ... [https://imerit.net/resources/blog/top-annotation-and-data-service-providers-for-clinical-trial-and-rwe-ai-in-2025/]
- 42. 36 Top RWE Platforms in 2025 [https://www.mahalo.health/insights/top-real-world-evidence-rwe-platforms]
- 43. Real-world clinical multi-omics analyses reveal bifurcation of ER-independent and ER-dependent drug resistance to CDK4/6 inhibitors | Nature Communications [https://www.nature.com/articles/s41467-025-55914-x]
- 44. Real-World Evidence: A Primer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9815890/]
- 45. Types of biological | networks analysis of Network ... protein [https://www.ebi.ac.uk/training/online/courses/network-analysis-of-protein-interaction-data-an-introduction/types-of-biological-networks/]
- 46. - Protein (PPI) and complex diseases... protein interaction networks [https://pmc.ncbi.nlm.nih.gov/articles/PMC4017556/]
- 47. BiNA: a visual analytics tool for biological network data [https://pubmed.ncbi.nlm.nih.gov/24551056/]
- 48. BiNA: A Visual Analytics Tool for Biological | PLOS One Network Data [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0087397]
- 49. A survey of visualization tools for biological analysis network [https://biodatamining.biomedcentral.com/articles/10.1186/1756-0381-1-12]
- 50. The future of AI regulation in drug development: a comparative analysis [https://pubmed.ncbi.nlm.nih.gov/41221487/]
- 51. GPT-5 vs o3 vs 4o vs GPT-5 Pro — Benchmarks & Best Uses [https://www.getpassionfruit.com/blog/chatgpt-5-vs-gpt-5-pro-vs-gpt-4o-vs-o3-performance-benchmark-comparison-recommendation-of-openai-s-2025-models]
- 52. The Complete LLM Model Comparison Guide ( 2025 ): Top Models... [https://www.helicone.ai/blog/the-complete-llm-model-comparison-guide]
- 53. Enhancing randomized clinical trials with digital twins | npj Systems Biology and Applications [https://www.nature.com/articles/s41540-025-00592-0]
- 54. A new generative AI approach to predicting chemical reactions | MIT News | Massachusetts Institute of Technology [https://news.mit.edu/2025/generative-ai-approach-to-predicting-chemical-reactions-0903]
- 55. Generative AI for computational chemistry: A roadmap to predicting emergent phenomena - PubMed [https://pubmed.ncbi.nlm.nih.gov/41052337/]
- 56. The Future Of Drug Trials Might Be Virtual AI Patients [https://www.forbes.com/sites/torconstantino/2025/06/03/the-future-of-drug-trials-might-be-virtual-ai-patients/]
- 57. A New Regulatory Road in Clinical Trials: Digital Twins | Applied Clinical Trials Online [https://www.appliedclinicaltrialsonline.com/view/new-regulatory-road-clinical-trials-digital-twins]
- 58. Our Guide to Success in Preclinical Data Analysis [https://www.kolaido.com/the-key-to-robust-translational-results-in-preclinical-data-analysis/]
- 59. All You Need To Know About Pharmacovigilance - Biomapas [https://www.biomapas.com/all-you-need-to-know-about-pharmacovigilance/]
- 60. A day in the life of a pharmacovigilance case processor - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5654220/]
- 61. Exploring the complexities of disproportionality analysis in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12014456/]
- 62. General Principles of Preclinical Study Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7610693/]
- 63. Frontiers | Computational Approaches in Preclinical Studies on Drug Discovery and Development [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2020.00726/full]
- 64. Effective Integration : Strategies for Smooth Data Flow Techniques [https://www.numberanalytics.com/blog/effective-integration-techniques-strategies]
- 65. Frontiers | A Qualitative Study of Stakeholders’ Views on Pharmacovigilance System, Policy, and Coordination in Pakistan [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.891954/full]
- 66. : Causes and Consequences Electrode Fouling [https://www.numberanalytics.com/blog/electrode-fouling-causes-consequences]
- 67. Recent strategies to minimise fouling in electrochemical detection... [https://researchers.mq.edu.au/en/publications/recent-strategies-to-minimise-fouling-in-electrochemical-detectio]
- 68. Improving the analysis of phase-separated bio-fuel samples with... [https://pubs.rsc.org/en/content/articlehtml/2024/ay/d4ay01006j]
- 69. Recommended strategies for spectral processing and post-processing of 1D 1H-NMR data of biofluids with a particular focus on urine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5809546/]
- 70. Quantitative 1H NMR spectroscopy - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0165993612000702]
- 71. in Electrocoagulation by Means of... Mitigating Electrode Fouling [https://pubmed.ncbi.nlm.nih.gov/33784607/]
- 72. NMR-Solver: Automated Structure Elucidation via Large-Scale Spectral Matching and Physics-Guided Fragment Optimization [https://arxiv.org/html/2509.00640v1]
- 73. Quantitative NMR in the spectroscopy evaluation of active... quality [https://www.spectroscopyeurope.com/article/quantitative-nmr-spectroscopy-quality-evaluation-active-pharmaceutical-ingredients-and]
- 74. Addressing AI : Strategies Companies Must Adopt Now Bias [https://www.forbes.com/councils/forbestechcouncil/2025/03/10/addressing-ai-bias-strategies-companies-must-adopt-now/]
- 75. [2506.08916] Enhancing of generalizability discovery across... model [https://arxiv.org/abs/2506.08916]
- 76. Ethical AI in 2025 : Auditing Models for Bias with Hugging... | Markaicode [https://markaicode.com/hugging-face-bias-audit-toolkit-2025/]
- 77. New benchmarks could help make AI less models biased [https://www.technologyreview.com/2025/03/11/1113000/these-new-ai-benchmarks-could-help-make-models-less-biased/]
- 78. Optimization Techniques for AI Performance in Model Enhanced 2025 [https://www.netguru.com/blog/ai-model-optimization]
- 79. Children’s drug research and development incentives and market pricing optimization based on medical imaging | Scientific Reports [https://www.nature.com/articles/s41598-025-22867-6]
- 80. and protocol assistance | European Medicines... Scientific advice [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-advice-protocol-assistance]
- 81. 5 FDA and EMA Collaboration | Regulatory Processes for Rare Disease Drugs in the United States and European Union: Flexibilities and Collaborative Opportunities | The National Academies Press [https://nap.nationalacademies.org/read/27968/chapter/7]
- 82. and FDA Regulatory Guidelines: A EMA Overview Comparative [https://www.linkedin.com/pulse/fda-ema-regulatory-guidelines-comparative-overview-chandrasekaran-w96vc]
- 83. EMA/FDA analysis shows high degree of alignment in marketing application decisions between EU and US | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/news/ema-fda-analysis-shows-high-degree-alignment-marketing-application-decisions-between-eu-and-us]
- 84. Challenges and ongoing initiatives towards better integrated EU scientific advice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808126/]
- 85. New FDA Guidance Aims to Simplify the Biosimilar Approval Process [https://www.goodwinlaw.com/en/insights/blogs/2025/11/new-fda-guidance-aims-to-simplify-the-biosimilar-approval-process]
- 86. The New Era of Biosimilar Development | Science Hub | Mabion [https://www.mabion.eu/science-hub/articles/the-new-era-of-biosimilar-development/]
- 87. Fiscal Year 2025 Generic Drug and Research... | Science FDA [https://www.fda.gov/drugs/news-events-human-drugs/fiscal-year-2025-generic-drug-science-and-research-initiatives-public-workshop-06032025]
- 88. Pharmaceutical Research and Development [https://www.pharmafocusamerica.com/strategy/pharmaceutical-research-and-development-the-power-of-collaborations]
- 89. 4 Key Tips for Workflow — CMW Lab Blog Coordination [https://www.cmwlab.com/blog/4-key-tips-workflow-coordination/]
- 90. Serverless Workflow Engines: 40+ Tools Ranked by Latency, Cost, and Developer Experience - DEV Community [https://dev.to/yigit-konur/serverless-workflow-engines-40-tools-ranked-by-latency-cost-and-developer-experience-19h2]
- 91. for Best - Practices Collaboration in Cross ... Functional Team Data [https://www.linkedin.com/pulse/best-practices-cross-functional-team-collaboration-mahwish-siddiqui-t2taf]
- 92. Effective Cross - Functional Coordination in Business... Team [https://datacalculus.com/en/knowledge-hub/business-intelligence/action-implementation/cross-functional-team-coordination]
- 93. The Winning Formula: Cross-Functional Collaboratio... [https://medicalaffairsspecialist.org/blog/the-winning-formula-cross-functional-collaboration-as-a-catalyst]
- 94. Top 5 Emerging Trends in Nanotechnology for 2025 [https://www.azonano.com/article.aspx?ArticleID=6865]
- 95. 6 trends shaping robotics and AI - The Robot Report [https://www.therobotreport.com/6-trends-shaping-robotics-and-ai/]
- 96. How to Validate in AI Applications for Life Science Companies GxP [https://fivevalidation.com/how-to-validate-ai/]
- 97. GxP Validation Process: What It Is And How to Implement It [https://www.sware.com/blog/gxp-validation-process]
- 98. Regulatory & Legal AI for Biopharma in Frameworks 2025 [https://intuitionlabs.ai/articles/ai-biopharma-regulation-2025]
- 99. and GxP : Compliance, AI and... | EY - Switzerland tools Validation [https://www.ey.com/en_ch/insights/life-sciences/gxp-and-ai-tools-compliance-validation-and-trust-in-pharma]
- 100. A guide to building AI agents in GxP environments | Artificial Intelligence [https://aws.amazon.com/blogs/machine-learning/a-guide-to-building-ai-agents-in-gxp-environments/]
- 101. GAMP 5: Computerized System Validation in Pharma | IntuitionLabs [https://intuitionlabs.ai/articles/gamp-5-computerized-system-validation-pharma]
- 102. EMA & FDA: What Are the Similarities & Differences in Risk Management Procedures? - Biomapas [https://www.biomapas.com/ema-and-fda-risk-management/]
- 103. FDA and EMA inspections: Similarities and Differences | Scilife [https://www.scilife.io/blog/fda-and-ema-inspections-pharma]
- 104. Navigating Regulatory Landscapes - FDA , EMA , & MHRA [https://careers.iconplc.com/blogs/2025-5/navigating-regulatory-landscapes-fda-ema-mhra]
- 105. FDA and EMA Resources, Policies, and Programs Relevant for Drug Development for Rare Diseases and Conditions - Regulatory Processes for Rare Disease Drugs in the United States and European Union - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK609376/]
- 106. FDA clinical trial phases and last approval steps | ZeClinics [https://www.zeclinics.com/blog/clinical-trial-phases-fda-approval/]
- 107. Duality of Risk-based Monitoring Definition: EMA vs FDA | Cyntegrity [https://cyntegrity.com/duality-risk-based-monitoring-definition-ema-vs-fda/]
- 108. ICH E6(R3) Explained: A Guide to the 2025 GCP Update | IntuitionLabs [https://intuitionlabs.ai/articles/ich-e6-r3-gcp-guidelines-2025]
- 109. Cancer drug applications to the EMA and the FDA: A comparison of new drugs and extension of indication in terms of approval decisions and time in review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12035586/]
- 110. and FDA : Key Differences in EMA Approval and Research Impact Drug [https://www.bioaccessla.com/blog/fda-and-ema-key-differences-in-drug-approval-and-research-impact]
- 111. Precision, Recall, Sensitivity and Specificity [https://iq.opengenus.org/precision-recall-sensitivity-specificity/]
- 112. and Sensitivity - Wikipedia specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 113. and Sensitivity Calculator Specificity [https://www.omnicalculator.com/statistics/sensitivity-and-specificity]
- 114. Innovative applications and future perspectives of chromatography-mass spectrometry in drug research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11979114/]
- 115. High-throughput high-performance liquid chromatography/mass spectrometry for modern drug discovery - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0958166900001762]
- 116. Sensitivity Enhancement for Separation-Based Analytical Techniques Utilizing Solid-Phase Enrichment Approaches and Analyte Derivatization for Trace Analysis in Various Matrices [https://www.mdpi.com/2297-8739/10/6/351]
- 117. Assessment of clinical analytical sensitivity and specificity of next-generation sequencing for detection of simple and complex mutations - PubMed [https://pubmed.ncbi.nlm.nih.gov/23418865/]
- 118. Assessment of clinical analytical sensitivity and specificity of next-generation sequencing for detection of simple and complex mutations | BMC Genomic Data | Full Text [https://bmcgenomdata.biomedcentral.com/articles/10.1186/1471-2156-14-6]
- 119. PCR Techniques in Next-Generation Sequencing - PubMed [https://pubmed.ncbi.nlm.nih.gov/26843053/]
- 120. A practical guide for choosing an optimal spatial transcriptomics... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11235-3]
- 121. Frontiers | Leveraging real-world data for safety signal detection and risk management in pre- and post-market settings [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2025.1626822/full]
- 122. What to expect in the clinical trials industry in [https://www.viedoc.com/blog/what-to-expect-clinical-trials-2025]
- 123. ICH Guidelines Explained: Global Harmonization for Drug Development [https://synapse.patsnap.com/article/ich-guidelines-explained-global-harmonization-for-drug-development]
- 124. A New Era for Clinical Trials: The ICH E6(R3) Guideline 2025 - Integra IT [https://www.integrait.co/a-new-era-for-clinical-trials-the-ich-e6r3-guideline-2025/]
- 125. - Real : Best Practices for Successful World ... Evidence Regulatory [https://acrpnet.org/2025/02/14/real-world-evidence-best-practices-for-successful-regulatory-engagements]
- 126. Legal Frameworks for Artificial Intelligence in Drug Discovery [https://natlawreview.com/article/ai-drug-discovery-2025-outlook]
- 127. Exploring socioeconomic and environmental coordination in the Yangtze River Delta Region using a game theory stepwise-cluster factorial coupling coordination model | Scientific Reports [https://www.nature.com/articles/s41598-024-77707-w]
- 128. Research on the coupling coordination, spatiotemporal evolution and zoning management of high-quality development and ecosystem service value in China | Scientific Reports [https://www.nature.com/articles/s41598-025-96627-x]
- 129. Patents in Pharma: Ranking the Top 25 Companies ( AI ) 2025 [https://intuitionlabs.ai/articles/pharma-ai-patent-leaders]
- 130. Cortellis Regulatory Intelligence AI -Powered Software [https://clarivate.com/life-sciences-healthcare/research-development/regulatory-compliance-intelligence/regulatory-intelligence-solutions/]